Data presentations highlight BMS’ leadership
and commitment to harnessing the full potential of cell therapy,
with advances in blood cancers and beyond
Multiple analyses underscore durable
efficacy and well-established safety profile of Breyanzi®
(lisocabtagene maraleucel; liso-cel) in leukemia and several types
of lymphoma
Expanded pipeline data across multiple
modalities feature first survival results for a GPRC5D-directed CAR
T, arlocabtagene autoleucel (arlo-cel; BMS-986393), and updated
results from a Phase 1 study reinforcing potential of CD19 NEX-T®
(BMS-986353) to deliver immune ‘reset’ among patients with severe
refractory lupus
Bristol Myers Squibb (NYSE: BMY) announced results from 18
presentations reinforcing its leadership in cell therapy, with data
demonstrating efficacy, durability and safety of currently
available therapies in blood cancers and highlighting the potential
of its pipeline for future indications including autoimmune
diseases. These results, covering a breadth of potential targets
within an expanding range of disease areas, were presented at the
66th American Society of Hematology (ASH) Annual Meeting and
Exposition in San Diego, California.
“Cell therapy is one of the fastest-growing modalities across
our industry, and we’re committed to unlocking its full potential
to deliver transformative treatments to patients with cancer and
beyond,” said Anne Kerber, senior vice president, head of late
clinical development, Hematology, Oncology and Cell Therapy (HOCT),
Bristol Myers Squibb. “Our data on Breyanzi and Abecma at ASH
reaffirm how our approved CAR T cell therapies continue to
demonstrate favorable long-term outcomes, while results from our
pipeline offer potential to address the unmet needs of patients
with relapsed or refractory multiple myeloma and severe refractory
autoimmune diseases.”
Key presentations include:
- Long-term analyses reinforcing the durable efficacy and
well-established safety profile of Breyanzi® (lisocabtagene
maraleucel; liso-cel) in large B-cell lymphoma (LBCL), follicular
lymphoma (FL) and chronic lymphocytic leukemia (CLL)/small
lymphocytic lymphoma (SLL)
- New circulating tumor DNA (ctDNA) data from the Phase 3
TRANSFORM study supporting the superiority of Breyanzi to achieve
deeper responses over the former standard of care in second-line
LBCL
- New analysis highlighting global manufacturing capability,
reliability and timely delivery for Abecma® (idecabtagene
vicleucel; ide-cel) in relapsed or refractory multiple myeloma
(RRMM)
- First overall and progression-free survival data for
arlocabtagene autoleucel (arlo-cel; BMS-986393), a GPRC5D-directed
CAR T cell therapy in RRMM
- Updated Phase 1 data for CD19 NEX-T® CAR T cell therapy
(BMS-986353/CC-97540), highlighting its potential to make a
meaningful impact for patients with severe, refractory autoimmune
diseases including systemic lupus erythematosus, systemic
sclerosis, idiopathic inflammatory myopathies, and multiple
sclerosis
“We’re excited to disclose the progress of our robust pipeline,
with promising early survival results for our GPRC5D-targeted cell
therapy underscoring the first-in-class potential of arlocabtagene
autoleucel for patients with relapsed or refractory multiple
myeloma,” said Bryan Campbell, senior vice president, Head of
Global Program Leaders, HOCT, Bristol Myers Squibb. “Beyond blood
cancers, we’re encouraged by the continued results we are seeing
with CD19 NEX-T in autoimmune diseases, like severe lupus,
highlighting its possibility as a one-time treatment to provide
sustained and treatment-free remission.”
Breyanzi Phase 1 TRANSCEND NHL Study Results:
Abstract #3125 Five-year overall survival (OS) data from the
Phase 1 TRANSCEND NHL 001 study support the deep and durable
responses of Breyanzi in patients with relapsed or refractory LBCL
(R/R LBCL) with median OS of 27.5 months (95% CI: 16.2–47.3) and an
estimated OS rate at 5 years of 38% (95% CI: 32-45), with patients
who achieved a complete response (CR) having the longest OS. The
median disease-specific survival (DSS) was 67.8 months (95% CI:
23.5 - not reached) and estimated DSS rate at 5 years was 52% (95%
CI: 45-59). Breyanzi continued to demonstrate an established safety
profile with no new safety signals.
Breyanzi Phase 3 TRANSFORM Study Results: Abstract
#72 New ctDNA data from the Phase 3 TRANSFORM study support
ctDNA as an early predictor of durable clinical benefit after
second-line LBCL treatment with Breyanzi. Patients with
undetectable ctDNA in the Breyanzi vs standard of care (SOC) arm
had longer event-free survival (EFS) at all predefined time points
and had statistically longer EFS at Day 126 which corresponds to
post-transplant visit for SOC arm (SOC vs Breyanzi: HR, 3.89 [95%
CI: 1.43–10.58]). Among patients who achieved both CR and
undetectable ctDNA at Day 126 in the study, Breyanzi provided
significantly greater EFS benefit vs SOC (SOC vs Breyanzi in
patients with CR and undetectable ctDNA: HR, 6.68 [95% CI:
2.11‒21.19]), supporting a deeper and more durable response with
Breyanzi vs SOC. These data underscore the role of ctDNA as a
biomarker of response in LBCL and support the superiority of
Breyanzi to achieve deeper responses over SOC in second-line
LBCL.
Breyanzi Real-World Outcomes in Second-Line LBCL:
Abstract #470 and Abstract #472 Real-world
data from the Center for International Blood and Marrow Transplant
Research (CIBMTR) Registry supported the use of Breyanzi as a
second-line salvage therapy and autologous stem cell transplant in
R/R LBCL regardless of age, including for younger (under 70 years)
and older patients (70 years and older). At a median follow-up of
6.4 months (95% CI: 6.1-6.5; range, 0.2-14.8), overall response
rate (ORR) and CR rate in the overall cohort (n=156) were 84% (95%
CI: 77–89) and 70% (95% CI: 62-77), respectively.
TRANSFORM-ineligible patients (n=105) had an ORR of 84% (95% CI:
75-90) and CR rate of 68% (95% CI: 58–76), while those who might
have been eligible (n=51) had an ORR of 84% (95% CI: 71–93) and CR
rate of 75% (95% CI: 60-86). Median duration of response (DOR),
progression-free survival (PFS), and OS were not reached. The
safety profile remained predictable, with cytokine release syndrome
(CRS) and immune effector cell–associated neurotoxicity syndrome
(ICANS) reported in 45% and 20% of patients, respectively.
Additionally, real-world data from the CIBMTR Registry supported
the use of Breyanzi as a feasible and effective therapeutic option
in real-world patients with R/R LBCL and secondary Central Nervous
System (sCNS) involvement. At a median follow up of 12 months (95%
CI: 1-24), ORR was 73% (95% CI: 60%–84%) and the CR rate was 64%
(95% CI: 50%–77%). The CR rate in this population was similar to
that observed in the overall population in the TRANSCEND NHL 001
(NCT02631044) study despite all patients in this study having sCNS
involvement. The safety profile of Breyanzi in patients with sCNS
was manageable and consistent with pivotal trials and prior
real-world reports. CRS, mostly low grade, was reported in 60% of
patients, and 58% did not experience any ICANS.
Breyanzi Phase 2 TRANSCEND FL Study Results:
Abstract #4387 After two years of follow-up, patients with
third-line-plus and second-line high-risk relapsed or refractory
follicular lymphoma (R/R FL) who received a single administration
of Breyanzi had ORR and CR rates above 94%. For third-line-plus
patients, 24-month DOR, PFS and OS were 74.6% (95% CI: 64.8-82.1),
72.5% (95% CI: 62.7-80.1), and 88.2% (95% CI: 80.1-93.1),
respectively. For 2L patients, 24-month DOR, PFS and OS were 86.4%
(95% CI: 63.4-95.4), 82.6% (95% CI: 60.1-90.3), and 95.7% (95% CI:
72.9-99.4), respectively. Breyanzi continued to demonstrate a
safety profile consistent with the primary analysis, with no new
safety signals. These data support Breyanzi as a durable and safe
treatment option for patients with R/R FL.
Breyanzi Phase 1/2 TRANSCEND CLL 004 Study Results:
Abstract #887 Primary analysis results from the Breyanzi
plus ibrutinib combination cohort of the Phase 1/2 TRANSCEND CLL
004 trial showed that treatment with Breyanzi plus ibrutinib, a
Bruton tyrosine kinase inhibitor (BTKi), resulted in deep
remissions (86% ORR [95% CI: 74-94], 45% CR [95% CI: 31-60] rate,
and 86% undetectable measurable residual disease (MRD) [95% CI:
74-94] rate in blood), as well as an established safety profile in
patients with R/R CLL/SLL. Grade ≥ 3 treatment emergent adverse
events (TEAEs) occurred in 48 (86%) of patients, most commonly
neutropenia (52%) and anemia (41%), with no Grade 5 TEAEs. The data
support this novel combination as a promising therapeutic strategy
for patients with R/R CLL/SLL.
Global Manufacturing Results for
Abecma: Abstract #3476 A new analysis of 4,117
RRMM patients who underwent leukapheresis for commercial Abecma
between February 23, 2021, and May 1, 2024, as captured on the Cell
Therapy 360® portal, found that the overall manufacturing success
rate (MSR) for Abecma was 96.8% and that the MSR rate improved over
3 years (95.8%, 96.4%, 97.2%, and 98.0% in 2021, 2022, 2023 and
2024, respectively). In addition, the analysis showed consistency
in commercial MSR across geographies in 2024 (97.7%, 98.3% and
98.0% in the US, EU and Japan, respectively). These results
reinforce the commercial manufacturing reliability for Abecma and
ability to meet the increasing global patient demand.
First Disclosure of Phase 1 Efficacy
and Safety Results of arlocabtagene autoleucel
(BMS-986393): Abstract #922 In an oral
presentation, BMS showcased the first OS and progression-free
survival (PFS) data for arlo-cel, a GPRC5D-targeted CAR T therapy.
In the Phase 1 study, patients had three or more prior
anti-multiple myeloma regimens including a proteasome inhibitor, an
immunomodulatory agent, and anti-CD38 therapy. After a median
follow-up of 16.1 months (range, 2.8-25.2) in efficacy-evaluable
patients (n= 79), arlo-cel demonstrated durable responses, with ORR
maintained at 87%. MRD was evaluated as an exploratory endpoint,
and 57% (48/84) of patients were MRD-evaluable. Results showed that
46% (22/48) of patients were MRD-negative and had a CR/stringent CR
(sCR). In all treated patients, 27% (23/84) were MRD-negative and
achieved a CR. Median PFS was 18.3 months (95% CI: 11.8-21.9) and
median OS was not reached. Treatment-related adverse events
(TRAEs), specifically hematological adverse events (AEs), were most
common in patients, with neutropenia occurring in 62 (74%)
patients. Overall, 69 patients (82%) had CRS. Three patients had
macrophage activation syndrome/hemophagocytic lymphohistiocytosis,
and ICANS occurred in eight patients. Safety data showed
on-target/off-tumor AEs were low frequency, low severity, and
mostly self-resolving.
These data support arlo-cel being investigated as a potential
first-in-class treatment for heavily pretreated RRMM and its
ongoing evaluation in the Phase 2 QUINTESSENTIAL study
(NCT06297226).
Updated Data of Phase 1 Study of
CD19-Directed CAR T BMS-986353: Abstract #2088
Updated data were presented from a Phase 1 study of CD19 NEX-T
(BMS-986353) highlighting the promising efficacy and safety in
patients with severe, refractory autoimmune diseases. Safety
results were presented for 17 patients, including 2 patients with
relapsing-remitting multiple sclerosis (MS), 3 patients with system
sclerosis (SSc), 1 patient with idiopathic inflammatory myopathies
(IIM), and 11 patients with systemic lupus erythematosus (SLE). In
efficacy-evaluable patients with SLE (n=7), significant
improvements in Systemic Lupus Erythematosus Disease Activity Index
(median score reduction of 10 points at 1 month following
BMS-986353 infusion) and Physician Global Assessment (median score
reduction of 82% at 1 month following BMS-986353 infusion) were
observed, and all patients remained off all autoimmune-directed
therapies without evidence of disease flare. Results showed
manageable initial safety in patients with autoimmune diseases. CRS
was reported in 1 patient with SLE (Grade 1) and 1 patient with SSc
(Grade 2), for a duration of one day. ICANS was reported in 1
patient with SSC (Grade 1) and 1 patient with SLE (Grade 3), with a
median duration of 3 days. There were no prolonged Grade ≥3
cytopenias or dose-limiting toxicities reported.
These results highlight the potential of BMS-986353 as a
one-time infusion of CD19-directed CAR T cell therapy to reset the
immune systems of patients with autoimmune diseases, which may
provide treatment-free sustained remission.
Bristol Myers Squibb thanks the patients and investigators
participating in these cell therapy clinical trials.
Please see the Important Safety Information section below,
including Boxed WARNINGS for Breyanzi and Abecma.
About TRANSCEND NHL 001
TRANSCEND NHL 001 (NCT02631044) is an open-label, multicenter,
pivotal, Phase 1, single-arm, seamless-design study to determine
the safety, pharmacokinetics and antitumor activity of Breyanzi in
patients with relapsed or refractory B-cell non-Hodgkin lymphoma,
including diffuse large B-cell lymphoma, high-grade B-cell
lymphoma, primary mediastinal B-cell lymphoma, follicular lymphoma
Grade 3B and mantle cell lymphoma. The primary outcome measures are
treatment-related adverse events, dose-limiting toxicities and
overall response rate. Secondary outcome measures include complete
response rate, duration of response, and progression-free
survival.
About TRANSFORM TRANSFORM
(NCT03575351) is a pivotal, global, randomized, multicenter Phase 3
trial evaluating Breyanzi compared to current standard therapy
regimens (platinum-based salvage chemotherapy followed by high-dose
chemotherapy and HSCT in patients responding to salvage
chemotherapy) in patients with large B-cell lymphoma (LBCL) that
was primary refractory or relapsed within 12 months after
CD20-antibody and anthracycline containing first-line therapy.
Patients were randomized to receive Breyanzi or standard of care
salvage therapy, including rituximab plus dexamethasone, high-dose
cytarabine, and cisplatin (R-DHAP), rituximab plus ifosfamide,
carboplatin and etoposide (R-ICE), or rituximab plus gemcitabine,
dexamethasone and cisplatin (R-GDP) per the investigators’ choice
before proceeding to high-dose chemotherapy (HDCT) and
hematopoietic stem cell transplant (HSCT). The primary endpoint of
the study was event-free survival (EFS), defined as time from
randomization to death from any cause, progressive disease, failure
to achieve complete response or partial response, or start of new
antineoplastic therapy due to efficacy concerns, whichever occurs
first. Complete response (CR) rate was a key secondary endpoint.
Other efficacy endpoints included progression-free survival (PFS),
overall survival (OS), overall response rate (ORR) and duration of
response (DOR).
About TRANSCEND CLL 004
TRANSCEND CLL 004 (NCT03331198) is a Phase 1/2 open-label,
single-arm, multicenter study evaluating Breyanzi in patients with
relapsed or refractory chronic lymphocytic leukemia or small
lymphocytic lymphoma. The Phase 1 dose escalation portion of the
study assessed the safety and recommended dose for the subsequent
Phase 2 expansion cohort. The phase 1 dose-escalation portion
includes cohorts assessing liso-cel monotherapy and liso-cel
combined with ibrutinib. The Phase 2 portion of the study is
evaluating Breyanzi at the recommended dose from the Phase 1
monotherapy arm. The primary endpoint of the Phase 2 portion of the
study is complete response rate, including complete remission with
incomplete bone marrow recovery, based on independent review
committee according to the International Workshop on Chronic
Lymphocytic Leukemia (iwCLL) 2018 guidelines.
About Breyanzi Breyanzi is a
CD19-directed CAR T cell therapy with a 4-1BB costimulatory domain,
which enhances the expansion and persistence of the CAR T cells.
Breyanzi is made from a patient’s own T cells, which are collected
and genetically reengineered to become CAR T cells that are then
delivered via infusion as a one-time treatment.
Breyanzi is approved in the U.S. for the treatment of relapsed
or refractory large B-cell lymphoma (LBCL) after at least one prior
line of therapy, and for the treatment of relapsed or refractory
chronic lymphocytic leukemia or small lymphocytic lymphoma after at
least two prior lines of therapy, and for the treatment of relapsed
or refractory follicular lymphoma in adult patients who have
received two or more prior lines of systemic therapy, and for the
treatment of relapsed or refractory mantle cell lymphoma in
patients who have received at least two prior lines of systemic
therapy, including a Bruton tyrosine kinase (BTK) inhibitor.
Breyanzi is also approved in Japan and Europe for the second-line
treatment of relapsed or refractory LBCL, and in Japan, Europe,
Switzerland and Canada for relapsed and refractory LBCL after two
or more lines of systemic therapy.
Bristol Myers Squibb’s clinical development program for Breyanzi
includes clinical studies in other types of lymphoma. For more
information, visit clinicaltrials.gov.
Indications BREYANZI is a
CD19-directed genetically modified autologous T cell immunotherapy
indicated for the treatment of:
- adult patients with large B-cell lymphoma (LBCL), including
diffuse large B-cell lymphoma (DLBCL) not otherwise specified
(including DLBCL arising from indolent lymphoma), high-grade B cell
lymphoma, primary mediastinal large B-cell lymphoma, and follicular
lymphoma grade 3B, who have:
- refractory disease to first-line chemoimmunotherapy or relapse
within 12 months of first-line chemoimmunotherapy; or
- refractory disease to first-line chemoimmunotherapy or relapse
after first-line chemoimmunotherapy and are not eligible for
hematopoietic stem cell transplantation (HSCT) due to comorbidities
or age; or
- relapsed or refractory disease after two or more lines of
systemic therapy.
Limitations of Use: BREYANZI is not
indicated for the treatment of patients with primary central
nervous system lymphoma.
- adult patients with relapsed or refractory chronic lymphocytic
leukemia (CLL) or small lymphocytic lymphoma (SLL) who have
received at least 2 prior lines of therapy, including a Bruton
tyrosine kinase (BTK) inhibitor and a B-cell lymphoma 2 (BCL-2)
inhibitor. This indication is approved under accelerated approval
based on response rate and duration of response. Continued approval
for this indication may be contingent upon verification and
description of clinical benefit in confirmatory trial(s).
- adult patients with relapsed or refractory follicular lymphoma
(FL) who have received 2 or more prior lines of systemic therapy.
This indication is approved under accelerated approval based on
response rate and duration of response. Continued approval for this
indication may be contingent upon verification and description of
clinical benefit in confirmatory trial(s).
- adult patients with relapsed or refractory mantle cell lymphoma
(MCL) who have received at least 2 prior lines of systemic therapy,
including a Bruton tyrosine kinase (BTK) inhibitor.
Important Safety Information
WARNING: CYTOKINE RELEASE SYNDROME, NEUROLOGIC TOXICITIES, AND
SECONDARY HEMATOLOGICAL MALIGNANCIES
- Cytokine Release Syndrome (CRS), including fatal or
life-threatening reactions, occurred in patients receiving
BREYANZI. Do not administer BREYANZI to patients with active
infection or inflammatory disorders. Treat severe or
life-threatening CRS with tocilizumab with or without
corticosteroids.
- Neurologic toxicities, including fatal or life-threatening
reactions, occurred in patients receiving BREYANZI, including
concurrently with CRS, after CRS resolution, or in the absence of
CRS. Monitor for neurologic events after treatment with BREYANZI.
Provide supportive care and/or corticosteroids as needed.
- T cell malignancies have occurred following treatment of
hematologic malignancies with BCMA- and CD19-directed genetically
modified autologous T cell immunotherapies, including
BREYANZI.
- BREYANZI is available only through a restricted program
under a Risk Evaluation and Mitigation Strategy (REMS) called the
BREYANZI REMS.
Cytokine Release Syndrome Cytokine release syndrome
(CRS), including fatal or life-threatening reactions, occurred
following treatment with BREYANZI. In clinical trials of BREYANZI,
which enrolled a total of 702 patients with non-Hodgkin lymphoma
(NHL), CRS occurred in 54% of patients, including ≥ Grade 3 CRS in
3.2% of patients. The median time to onset was 5 days (range: 1 to
63 days). CRS resolved in 98% of patients with a median duration of
5 days (range: 1 to 37 days). One patient had fatal CRS and 5
patients had ongoing CRS at the time of death. The most common
manifestations of CRS (≥10%) were fever, hypotension, tachycardia,
chills, hypoxia, and headache.
Serious events that may be associated with CRS include cardiac
arrhythmias (including atrial fibrillation and ventricular
tachycardia), cardiac arrest, cardiac failure, diffuse alveolar
damage, renal insufficiency, capillary leak syndrome, hypotension,
hypoxia, and hemophagocytic lymphohistiocytosis/macrophage
activation syndrome (HLH/MAS).
Ensure that 2 doses of tocilizumab are available prior to
infusion of BREYANZI.
Neurologic Toxicities
Neurologic toxicities that were fatal or life-threatening,
including immune effector cell-associated neurotoxicity syndrome
(ICANS), occurred following treatment with BREYANZI. Serious events
including cerebral edema and seizures occurred with BREYANZI. Fatal
and serious cases of leukoencephalopathy, some attributable to
fludarabine, also occurred.
In clinical trials of BREYANZI, CAR T cell-associated neurologic
toxicities occurred in 31% of patients, including ≥ Grade 3 cases
in 10% of patients. The median time to onset of neurotoxicity was 8
days (range: 1 to 63 days). Neurologic toxicities resolved in 88%
of patients with a median duration of 7 days (range: 1 to 119
days). Of patients developing neurotoxicity, 82% also developed
CRS.
The most common neurologic toxicities (≥5%) included
encephalopathy, tremor, aphasia, headache, dizziness, and
delirium.
CRS and Neurologic Toxicities Monitoring
Monitor patients daily for at least 7 days following BREYANZI
infusion at a REMS-certified healthcare facility for signs and
symptoms of CRS and neurologic toxicities and assess for other
causes of neurological symptoms. Monitor patients for signs and
symptoms of CRS and neurologic toxicities for at least 4 weeks
after infusion and treat promptly. At the first sign of CRS,
institute treatment with supportive care, tocilizumab, or
tocilizumab and corticosteroids as indicated. Manage neurologic
toxicity with supportive care and/or corticosteroid as needed.
Counsel patients to seek immediate medical attention should signs
or symptoms of CRS or neurologic toxicity occur at any time.
BREYANZI REMS
Because of the risk of CRS and neurologic toxicities, BREYANZI
is available only through a restricted program under a Risk
Evaluation and Mitigation Strategy (REMS) called the BREYANZI REMS.
The required components of the BREYANZI REMS are:
- Healthcare facilities that dispense and administer BREYANZI
must be enrolled and comply with the REMS requirements.
- Certified healthcare facilities must have on-site, immediate
access to tocilizumab.
- Ensure that a minimum of 2 doses of tocilizumab are available
for each patient for infusion within 2 hours after BREYANZI
infusion, if needed for treatment of CRS.
Further information is available at www.BreyanziREMS.com, or
contact Bristol Myers Squibb at 1-866-340-7332.
Hypersensitivity Reactions
Allergic reactions may occur with the infusion of BREYANZI.
Serious hypersensitivity reactions, including anaphylaxis, may be
due to dimethyl sulfoxide (DMSO).
Serious Infections
Severe infections, including life-threatening or fatal
infections, have occurred in patients after BREYANZI infusion. In
clinical trials of BREYANZI, infections of any grade occurred in
34% of patients, with Grade 3 or higher infections occurring in 12%
of all patients. Grade 3 or higher infections with an unspecified
pathogen occurred in 7%, bacterial infections in 3.7%, viral
infections in 2%, and fungal infections in 0.7% of patients. One
patient who received 4 prior lines of therapy developed a fatal
case of John Cunningham (JC) virus progressive multifocal
leukoencephalopathy 4 months after treatment with BREYANZI. One
patient who received 3 prior lines of therapy developed a fatal
case of cryptococcal meningoencephalitis 35 days after treatment
with BREYANZI.
Febrile neutropenia developed after BREYANZI infusion in 8% of
patients. Febrile neutropenia may be concurrent with CRS. In the
event of febrile neutropenia, evaluate for infection and manage
with broad-spectrum antibiotics, fluids, and other supportive care
as medically indicated.
Monitor patients for signs and symptoms of infection before and
after BREYANZI administration and treat appropriately. Administer
prophylactic antimicrobials according to standard institutional
guidelines. Avoid administration of BREYANZI in patients with
clinically significant, active systemic infections.
Viral reactivation: Hepatitis B virus (HBV) reactivation, in
some cases resulting in fulminant hepatitis, hepatic failure, and
death, can occur in patients treated with drugs directed against B
cells. In clinical trials of BREYANZI, 35 of 38 patients with a
prior history of HBV were treated with concurrent antiviral
suppressive therapy. Perform screening for HBV, HCV, and HIV in
accordance with clinical guidelines before collection of cells for
manufacturing. In patients with prior history of HBV, consider
concurrent antiviral suppressive therapy to prevent HBV
reactivation per standard guidelines.
Prolonged Cytopenias
Patients may exhibit cytopenias not resolved for several weeks
following lymphodepleting chemotherapy and BREYANZI infusion. In
clinical trials of BREYANZI, Grade 3 or higher cytopenias persisted
at Day 29 following BREYANZI infusion in 35% of patients, and
included thrombocytopenia in 25%, neutropenia in 22%, and anemia in
6% of patients. Monitor complete blood counts prior to and after
BREYANZI administration.
Hypogammaglobulinemia
B-cell aplasia and hypogammaglobulinemia can occur in patients
receiving BREYANZI. In clinical trials of BREYANZI,
hypogammaglobulinemia was reported as an adverse reaction in 10% of
patients. Hypogammaglobulinemia, either as an adverse reaction or
laboratory IgG level below 500 mg/dL after infusion, was reported
in 30% of patients. Monitor immunoglobulin levels after treatment
with BREYANZI and manage using infection precautions, antibiotic
prophylaxis, and immunoglobulin replacement as clinically
indicated.
Live vaccines: The safety of immunization with live viral
vaccines during or following BREYANZI treatment has not been
studied. Vaccination with live virus vaccines is not recommended
for at least 6 weeks prior to the start of lymphodepleting
chemotherapy, during BREYANZI treatment, and until immune recovery
following treatment with BREYANZI.
Secondary Malignancies
Patients treated with BREYANZI may develop secondary
malignancies. T cell malignancies have occurred following treatment
of hematologic malignancies with BCMA- and CD19-directed
genetically modified autologous T cell immunotherapies, including
BREYANZI. Mature T cell malignancies, including CAR-positive
tumors, may present as soon as weeks following infusion, and may
include fatal outcomes. Monitor lifelong for secondary
malignancies. In the event that a secondary malignancy occurs,
contact Bristol Myers Squibb at 1-888-805-4555 for reporting and to
obtain instructions on collection of patient samples for
testing.
Effects on Ability to Drive and Use Machines
Due to the potential for neurologic events, including altered
mental status or seizures, patients receiving BREYANZI are at risk
for developing altered or decreased consciousness or impaired
coordination in the 8 weeks following BREYANZI administration.
Advise patients to refrain from driving and engaging in hazardous
occupations or activities, such as operating heavy or potentially
dangerous machinery, for at least 8 weeks.
Immune Effector Cell-Associated Hemophagocytic
Lymphohistiocytosis-Like Syndrome (IEC-HS)
Immune Effector Cell-Associated Hemophagocytic
Lymphohistiocytosis-Like Syndrome (IEC-HS), including fatal or
life-threatening reactions, occurred following treatment with
BREYANZI. Three of 89 (3%) safety evaluable patients with R/R
CLL/SLL developed IEC-HS. Time to onset of IEC-HS ranged from 7 to
18 days. Two of the 3 patients developed IEC-HS in the setting of
ongoing CRS and 1 in the setting of ongoing neurotoxicity. IEC-HS
was fatal in 2 of 3 patients. One patient had fatal IEC-HS and one
had ongoing IEC-HS at time of death. IEC-HS is a life-threatening
condition with a high mortality rate if not recognized and treated
early. Treatment of IEC-HS should be administered per current
practice guidelines.
Adverse Reactions
The most common adverse reaction(s) (incidence ≥30%) in:
- LBCL are fever, cytokine release syndrome, fatigue,
musculoskeletal pain, and nausea. The most common Grade 3-4
laboratory abnormalities include lymphocyte count decrease,
neutrophil count decrease, platelet count decrease, and hemoglobin
decrease.
- CLL/SLL are cytokine release syndrome, encephalopathy, fatigue,
musculoskeletal pain, nausea, edema, and diarrhea. The most common
Grade 3-4 laboratory abnormalities include neutrophil count
decrease, white blood cell decrease, hemoglobin decrease, platelet
count decrease, and lymphocyte count decrease.
- FL is cytokine release syndrome. The most common Grade 3-4
laboratory abnormalities include lymphocyte count decrease,
neutrophil count decrease, and white blood cell decrease.
- MCL are cytokine release syndrome, fatigue, musculoskeletal
pain, and encephalopathy. The most common Grade 3-4 laboratory
abnormalities include neutrophil count decrease, white blood cell
decrease, and platelet count decrease.
Please see full Prescribing Information,
including Boxed WARNINGS and Medication
Guide.
About Abecma Abecma is a
B-cell maturation antigen (BCMA)-directed genetically modified
autologous T cell immunotherapy indicated for the treatment of
adult patients with relapsed or refractory multiple myeloma after
two or more prior lines of therapy, including an immunomodulatory
agent, a proteasome inhibitor, and an anti-CD38 monoclonal
antibody. Abecma is being jointly developed and commercialized in
the U.S. as part of a Co-Development, Co-Promotion, and Profit
Share Agreement between Bristol Myers Squibb and 2seventy bio.
Abecma U.S. Indication
ABECMA (idecabtagene vicleucel) is a B-cell maturation antigen
(BCMA)-directed genetically modified autologous T cell
immunotherapy indicated for the treatment of adult patients with
relapsed or refractory multiple myeloma after two or more prior
lines of therapy, including an immunomodulatory agent, a proteasome
inhibitor, and an anti-CD38 monoclonal antibody.
U.S. Important Safety
Information
WARNING: CYTOKINE RELEASE SYNDROME, NEUROLOGIC TOXICITIES,
HLH/MAS, PROLONGED CYTOPENIA and SECONDARY HEMATOLOGICAL
MALIGNANCIES
- Cytokine Release Syndrome (CRS), including fatal or
life-threatening reactions, occurred in patients following
treatment with ABECMA. Do not administer ABECMA to patients with
active infection or inflammatory disorders. Treat severe or
life-threatening CRS with tocilizumab or tocilizumab and
corticosteroids.
- Neurologic Toxicities, which may be severe or life-threatening,
occurred following treatment with ABECMA, including concurrently
with CRS, after CRS resolution, or in the absence of CRS. Monitor
for neurologic events after treatment with ABECMA. Provide
supportive care and/or corticosteroids as needed.
- Hemophagocytic Lymphohistiocytosis/Macrophage Activation
Syndrome (HLH/MAS) including fatal and life-threatening reactions,
occurred in patients following treatment with ABECMA. HLH/MAS can
occur with CRS or neurologic toxicities.
- Prolonged Cytopenia with bleeding and infection, including
fatal outcomes following stem cell transplantation for
hematopoietic recovery, occurred following treatment with
ABECMA.
- T cell malignancies have occurred following treatment of
hematologic malignancies with BCMA- and CD19-directed genetically
modified autologous T cell immunotherapies, including ABECMA.
- ABECMA is available only through a restricted program under a
Risk Evaluation and Mitigation Strategy (REMS) called the ABECMA
REMS.
Warnings and Precautions:
Early Death: In KarMMa-3, a randomized (2:1), controlled
trial, a higher proportion of patients experienced death within 9
months after randomization in the ABECMA arm (45/254; 18%) compared
to the standard regimens arm (15/132; 11%). Early deaths occurred
in 8% (20/254) and 0% prior to ABECMA infusion and standard regimen
administration, respectively, and 10% (25/254) and 11% (15/132)
after ABECMA infusion and standard regimen administration,
respectively. Out of the 20 deaths that occurred prior to ABECMA
infusion, 15 occurred from disease progression, 3 occurred from
adverse events and 2 occurred from unknown causes. Out of the 25
deaths that occurred after ABECMA infusion, 10 occurred from
disease progression, 11 occurred from adverse events, and 4
occurred from unknown causes.
Cytokine Release Syndrome (CRS): CRS, including fatal or
life-threatening reactions, occurred following treatment with
ABECMA. Among patients receiving ABECMA for relapsed refractory
multiple myeloma in the KarMMa and KarMMa-3 studies (N=349), CRS
occurred in 89% (310/349), including ≥ Grade 3 CRS (Lee grading
system) in 7% (23/349) of patients and Grade 5 CRS in 0.9% (3/349)
of patients. The median time-to-onset of CRS, any grade, was 1 day
(range: 1 to 27 days), and the median duration of CRS was 5 days
(range: 1 to 63 days). In the pooled studies, the rate of ≥Grade 3
CRS was 10% (7/71) for patients treated in dose range of 460 to 510
x 106 CAR-positive T cells and 5.4% (13/241) for patients treated
in dose range of 300 to 460 x 106 CAR-positive T cells.
The most common manifestations of CRS (greater than or equal to
10%) included pyrexia (87%), hypotension (30%), tachycardia (26%),
chills (19%), hypoxia (16%). Grade 3 or higher events that may be
associated with CRS include hypotension, hypoxia,
hyperbilirubinemia, hypofibrinogenemia, ARDS, atrial fibrillation,
hepatocellular injury, metabolic acidosis, pulmonary edema,
coagulopathy, renal failure, multiple organ dysfunction syndrome
and HLH/MAS.
Identify CRS based on clinical presentation. Evaluate for and
treat other causes of fever, hypoxia, and hypotension. CRS has been
reported to be associated with findings of HLH/MAS, and the
physiology of the syndromes may overlap. HLH/MAS is a potentially
life-threatening condition. In patients with progressive symptoms
of CRS or refractory CRS despite treatment, evaluate for evidence
of HLH/MAS.
Of the 349 patients who received ABECMA in clinical trials, 226
(65%) patients received tocilizumab; 39% (135/349) received a
single dose, while 26% (91/349) received more than 1 dose of
tocilizumab. Overall, 24% (82/349) of patients received at least 1
dose of corticosteroids for treatment of CRS. Almost all patients
who received corticosteroids for CRS also received tocilizumab. For
patients treated in dose range of 460 to 510 x 106 CAR-positive T
cells, 76% (54/71) of patients received tocilizumab and 35% (25/71)
received at least 1 dose of corticosteroids for treatment of CRS.
For patients treated in dose range of 300 to 460 x 106 CAR-positive
T cells, 63% (152/241) of patients received tocilizumab and 20%
(49/241) received at least 1 dose of corticosteroid for treatment
of CRS.
Monitor patients at least daily for 7 days following ABECMA
infusion at the REMS-certified healthcare facility for signs or
symptoms of CRS and monitor patients for signs or symptoms of CRS
for at least 4 weeks after ABECMA infusion. At the first sign of
CRS, institute treatment with supportive care, tocilizumab and/or
corticosteroids as indicated. Ensure that a minimum of 2 doses of
tocilizumab are available prior to infusion of ABECMA. Counsel
patients to seek immediate medical attention should signs or
symptoms of CRS occur at any time.
Neurologic Toxicities: Neurologic toxicities, including
immune-effector cell-associated neurotoxicity (ICANS), which may be
severe or life- threatening, occurred concurrently with CRS, after
CRS resolution, or in the absence of CRS following treatment with
ABECMA.
In patients receiving ABECMA in the KarMMa and KarMMa-3 studies,
CAR T cell-associated neurotoxicity occurred in 40% (139/349),
including Grade 3 in 4% (14/349) and Grade 4 in 0.6% (2/349) of
patients. The median time to onset of neurotoxicity was 2 days
(range: 1 to 148 days). The median duration of CAR T
cell-associated neurotoxicity was 8 days (range: 1 to 720 days) in
all patients including those with ongoing neurologic events at the
time of death or data cut off. CAR T cell-associated neurotoxicity
resolved in 123 of 139 (88%) patients and median time to resolution
was 5 days (range: 1 to 245 days). One-hundred and thirty four out
of 349 (38%) patients with neurotoxicity had CRS. The onset of
neurotoxicity during CRS was observed in 93 patients, before the
onset of CRS in 12 patients, and after the CRS event in 29
patients. The rate of Grade 3 or 4 CAR T cell-associated
neurotoxicity was 5.6% (4/71) and 3.7% (9/241) for patients treated
in dose range of 460 to 510 x 106 CAR-positive T cells and 300 to
460 x 106 CAR-positive T cells, respectively. The most frequent
(greater than or equal to 5%) manifestations of CAR T
cell-associated neurotoxicity include encephalopathy (21%),
headache (15%), dizziness (8%), delirium (6%), and tremor (6%).
At the safety update for KarMMa-3 study, one patient developed
fatal neurotoxicity 43 days after ABECMA. In KarMMa, one patient
had ongoing Grade 2 neurotoxicity at the time of death. Two
patients had ongoing Grade 1 tremor at the time of data cutoff.
Cerebral edema has been associated with ABECMA in a patient in
another study in multiple myeloma. Grade 3 myelitis and Grade 3
parkinsonism have occurred after treatment with ABECMA in another
study in multiple myeloma.
Monitor patients at least daily for 7 days following ABECMA
infusion at the REMS-certified healthcare facility for signs or
symptoms of neurologic toxicities and monitor patients for signs or
symptoms of neurologic toxicities for at least 4 weeks after ABECMA
infusion and treat promptly. Rule out other causes of neurologic
symptoms. Neurologic toxicity should be managed with supportive
care and/or corticosteroids as needed. Counsel patients to seek
immediate medical attention should signs or symptoms occur at any
time.
Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage
Activation Syndrome (MAS): In patients receiving ABECMA in the
KarMMa and KarMMa-3 studies, HLH/MAS occurred in 2.9% (10/349) of
patients. All events of HLH/MAS had onset within 10 days of
receiving ABECMA, with a median onset of 6.5 days (range: 4 to 10
days) and occurred in the setting of ongoing or worsening CRS. Five
patients with HLH/MAS had overlapping neurotoxicity. The
manifestations of HLH/MAS include hypotension, hypoxia, multiple
organ dysfunction, renal dysfunction and cytopenia.
In KarMMa-3, one patient had Grade 5, two patients had Grade 4
and two patients had Grade 3 HLH/MAS. The patient with Grade 5
HLH/MAS also had Grade 5 candida sepsis and Grade 5 CRS. In another
patient who died due to stroke, the Grade 4 HLH/MAS had resolved
prior to death. Two cases of Grade 3 and one case of Grade 4
HLH/MAS had resolved.
In KarMMa, one patient treated in the 300 x 106 CAR-positive T
cells dose cohort developed fatal multi-organ HLH/MAS with CRS. In
another patient with fatal bronchopulmonary aspergillosis, HLH/MAS
was contributory to the fatal outcome. Three cases of Grade 2
HLH/MAS resolved.
HLH/MAS is a potentially life-threatening condition with a high
mortality rate if not recognized early and treated. Treatment of
HLH/MAS should be administered per institutional guidelines.
ABECMA REMS: Due to the risk of CRS and neurologic
toxicities, ABECMA is available only through a restricted program
under a Risk Evaluation and Mitigation Strategy (REMS) called the
ABECMA REMS. Further information is available at www.AbecmaREMS.com
or contact Bristol Myers Squibb at 1-866-340-7332.
Hypersensitivity Reactions: Allergic reactions may occur
with the infusion of ABECMA. Serious hypersensitivity reactions,
including anaphylaxis, may be due to dimethyl sulfoxide (DMSO) in
ABECMA.
Infections: ABECMA should not be administered to patients
with active infections or inflammatory disorders. Severe,
life-threatening, or fatal infections occurred in patients after
ABECMA infusion.
In all patients receiving ABECMA in the KarMMa and KarMMa-3
studies, infections (all grades) occurred in 61% of patients. Grade
3 or 4 infections occurred in 21% of patients. Grade 3 or 4
infections with an unspecified pathogen occurred in 12%, viral
infections in 7%, bacterial infections in 4.3%, and fungal
infections in 1.4% of patients. Overall, 15 patients had Grade 5
infections (4.3%); 8 patients (2.3%) with infections of pathogen
unspecified, 3 patients (0.9%) with fungal infections, 3 patients
(0.9%) with viral infections, and 1 patient (0.3%) with bacterial
infection.
Monitor patients for signs and symptoms of infection before and
after ABECMA infusion and treat appropriately. Administer
prophylactic, pre-emptive, and/or therapeutic antimicrobials
according to standard institutional guidelines.
Febrile neutropenia was observed in 38% (133/349) of patients
after ABECMA infusion and may be concurrent with CRS. In the event
of febrile neutropenia, evaluate for infection and manage with
broad-spectrum antibiotics, fluids, and other supportive care as
medically indicated.
Viral Reactivation: Cytomegalovirus (CMV) infection resulting in
pneumonia and death has occurred following ABECMA administration.
Monitor and treat for CMV reactivation in accordance with clinical
guidelines. Hepatitis B virus (HBV) reactivation, in some cases
resulting in fulminant hepatitis, hepatic failure, and death, can
occur in patients treated with drugs directed against plasma cells.
Perform screening for CMV, HBV, hepatitis C virus (HCV), and human
immunodeficiency virus (HIV) in accordance with clinical guidelines
before collection of cells for manufacturing. Consider antiviral
therapy to prevent viral reactivation per local institutional
guidelines/clinical practice.
Prolonged Cytopenias: In patients receiving ABECMA in the
KarMMa and KarMMa-3 studies, 40% of patients (139/349) experienced
prolonged Grade 3 or 4 neutropenia and 42% (145/349) experienced
prolonged Grade 3 or 4 thrombocytopenia that had not resolved by
Month 1 following ABECMA infusion. In 89% (123/139) of patients who
recovered from Grade 3 or 4 neutropenia after Month 1, the median
time to recovery from ABECMA infusion was 1.9 months. In 76%
(110/145) of patients who recovered from Grade 3 or 4
thrombocytopenia, the median time to recovery was 1.9 months. Five
patients underwent stem cell therapy for hematopoietic
reconstitution due to prolonged cytopenia. The rate of Grade 3 or 4
thrombocytopenia was 62% (44/71) and 56% (135/241) for patients
treated in dose range of 460 to 510 x 106 CAR-positive T cells and
300 to 460 x 106 CAR-positive T cells, respectively.
Monitor blood counts prior to and after ABECMA infusion. Manage
cytopenia with myeloid growth factor and blood product transfusion
support according to local institutional guidelines.
Hypogammaglobulinemia: In all patients receiving ABECMA
in the KarMMa and KarMMa-3 studies, hypogammaglobulinemia was
reported as an adverse event in 13% (46/349) of patients;
laboratory IgG levels fell below 500 mg/dL after infusion in 37%
(130/349) of patients treated with ABECMA.
Hypogammaglobulinemia either as an adverse reaction or
laboratory IgG level below 500 mg/dL after infusion occurred in 45%
(158/349) of patients treated with ABECMA. Forty-one percent of
patients received intravenous immunoglobulin (IVIG) post-ABECMA for
serum IgG <400 mg/dL.
Monitor immunoglobulin levels after treatment with ABECMA and
administer IVIG for IgG <400 mg/dl. Manage appropriately per
local institutional guidelines, including infection precautions and
antibiotic or antiviral prophylaxis.
Use of Live Vaccines: The safety of immunization with live viral
vaccines during or after ABECMA treatment has not been studied.
Vaccination with live virus vaccines is not recommended for at
least 6 weeks prior to the start of lymphodepleting chemotherapy,
during ABECMA treatment, and until immune recovery following
treatment with ABECMA.
Secondary Malignancies: Patients treated with ABECMA may
develop secondary malignancies. In KarMMa-3, myeloid neoplasms
(four cases of myelodysplastic syndrome and one case of acute
myeloid leukemia) occurred in 2.2% (5/222) of patients following
treatment with ABECMA compared to none in the standard regimens arm
at the time of the safety update. The median time to onset of
myeloid neoplasm from ide-cel infusion was 338 days (Range: 277 to
794 days). Three of these five patients have died following the
development of myeloid neoplasm. One out of the five cases of
myeloid neoplasm occurred after initiation of subsequent
antimyeloma therapy.
T cell malignancies have occurred following treatment of
hematologic malignancies with BCMA- and CD19-directed genetically
modified autologous T cell immunotherapies, including ABECMA.
Mature T cell malignancies, including CAR-positive tumors, may
present as soon as weeks following infusion, and may include fatal
outcomes.
Monitor life-long for secondary malignancies. In the event that
a secondary malignancy occurs, contact Bristol Myers Squibb at
18888054555 for reporting and to obtain instructions on collection
of patient samples for testing of secondary malignancy.
Effects on Ability to Drive and Operate Machinery: Due to
the potential for neurologic events, including altered mental
status or seizures, patients receiving ABECMA are at risk for
altered or decreased consciousness or coordination in the 8 weeks
following ABECMA infusion. Advise patients to refrain from driving
and engaging in hazardous occupations or activities, such as
operating heavy or potentially dangerous machinery, during this
initial period.
Adverse Reactions: The most common nonlaboratory adverse
reactions (incidence greater than or equal to 20%) include pyrexia,
CRS, hypogammaglobulinemia, infections – pathogen unspecified,
musculoskeletal pain, fatigue, febrile neutropenia, hypotension,
tachycardia, diarrhea, nausea, headache, chills, upper respiratory
tract infection, encephalopathy, edema, dyspnea and viral
infections.
Please see full Prescribing Information, including Boxed
WARNINGS and Medication Guide.
Bristol Myers Squibb: Unlocking the
Full Potential of Cell Therapy A pioneer in harnessing
the immune system to fight cancer and an established leader in cell
therapy, Bristol Myers Squibb is uniquely positioned to unlock the
full potential of this technology across blood cancers and within
new frontiers, including autoimmune disease.
Bristol Myers Squibb is currently the only company with two
approved CAR T cell therapies with two distinct targets, available
in major markets around the world. Our bold vision for the future
is one in which hundreds of thousands of patients can be treated
with cell therapy’s transformational potential.
The building blocks to realize this ambition—a promising and
differentiated pipeline, extensive translational and clinical data
sets, a deep bench of talent, and robust manufacturing
capabilities—are in our cells. We are laser-focused on advancing
the field of cell therapy toward a true revolution for patients.
Learn more about the science behind cell therapy and ongoing
progress at Bristol Myers Squibb here.
Bristol Myers Squibb: Creating a Better
Future for People with Cancer Bristol Myers Squibb is
inspired by a single vision—transforming patients’ lives through
science. The goal of the company’s cancer research is to deliver
medicines that offer each patient a better, healthier life and to
make cure a possibility. Building on a legacy across a broad range
of cancers that have changed survival expectations for many,
Bristol Myers Squibb researchers are exploring new frontiers in
personalized medicine, and through innovative digital platforms,
are turning data into insights that sharpen their focus. Deep
understanding of causal human biology, cutting-edge capabilities
and differentiated research platforms uniquely position the company
to approach cancer from every angle.
Cancer can have a relentless grasp on many parts of a patient’s
life, and Bristol Myers Squibb is committed to taking actions to
address all aspects of care, from diagnosis to survivorship. As a
leader in cancer care, Bristol Myers Squibb is working to empower
all people with cancer to have a better future.
Learn more about the science behind cell therapy and ongoing
research at Bristol Myers Squibb here.
About Bristol Myers Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose
mission is to discover, develop and deliver innovative medicines
that help patients prevail over serious diseases. For more
information about Bristol Myers Squibb, visit us at BMS.com or
follow us on LinkedIn, X, YouTube, Facebook and Instagram.
Cautionary Statement Regarding
Forward-Looking Statements This press release contains
“forward-looking statements” within the meaning of the Private
Securities Litigation Reform Act of 1995 regarding, among other
things, the research, development and commercialization of
pharmaceutical products. All statements that are not statements of
historical facts are, or may be deemed to be, forward-looking
statements. Such forward-looking statements are based on current
expectations and projections about our future financial results,
goals, plans and objectives and involve inherent risks, assumptions
and uncertainties, including internal or external factors that
could delay, divert or change any of them in the next several
years, that are difficult to predict, may be beyond our control and
could cause our future financial results, goals, plans and
objectives to differ materially from those expressed in, or implied
by, the statements. These risks, assumptions, uncertainties and
other factors include, among others, that future study results may
not be consistent with the results to date, that the products,
product candidates, treatments and combination treatments described
in this release may not receive regulatory approval for the
indications described in this release, any marketing approvals, if
granted, may have significant limitations on their use, and, if
approved, whether such products, product candidates, treatments and
combination treatments for such indications will be commercially
successful. No forward-looking statement can be guaranteed.
Forward-looking statements in this press release should be
evaluated together with the many risks and uncertainties that
affect Bristol Myers Squibb’s business and market, particularly
those identified in the cautionary statement and risk factors
discussion in Bristol Myers Squibb’s Annual Report on Form 10-K for
the year ended December 31, 2023, as updated by our subsequent
Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and
other filings with the Securities and Exchange Commission. The
forward-looking statements included in this document are made only
as of the date of this document and except as otherwise required by
applicable law, Bristol Myers Squibb undertakes no obligation to
publicly update or revise any forward-looking statement, whether as
a result of new information, future events, changed circumstances
or otherwise.
corporatefinancial-news
View source
version on businesswire.com: https://www.businesswire.com/news/home/20241206448024/en/
Bristol Myers Squibb
Media Inquiries: media@bms.com
Investors: investor.relations@bms.com
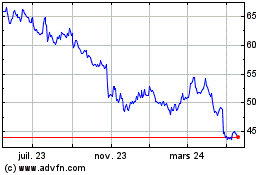
Bristol Myers Squibb (NYSE:BMY)
Graphique Historique de l'Action
De Nov 2024 à Déc 2024
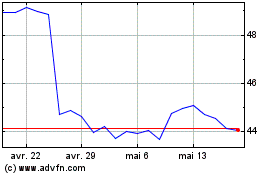
Bristol Myers Squibb (NYSE:BMY)
Graphique Historique de l'Action
De Déc 2023 à Déc 2024