Merck Underscores Continued Commitment to
Fighting Infectious Diseases with More than 40 Data Presentations
Across Vaccines, Antibacterials and Antivirals, Including
Respiratory Syncytial Virus, Pneumococcal Disease and HIV
For the First Time, Full Results will be
Highlighted from the Phase 2b/3 Trial of Clesrovimab (MK-1654), an
Investigational Respiratory Syncytial Virus Preventative Monoclonal
Antibody for Infants
Merck (NYSE: MRK), known as MSD outside of the United States and
Canada, today announced its plans to present new research findings
demonstrating the continued impact of its increasingly broad and
diverse vaccines and infectious disease portfolio and the potential
of its innovative pipeline at IDWeek 2024 in Los Angeles, CA, from
October 16-19.
Data to be presented include a late-breaker oral presentation of
positive detailed results from the Phase 2b/3 trial evaluating
clesrovimab (MK-1654), an investigational prophylactic monoclonal
antibody designed to protect infants from respiratory syncytial
virus (RSV) disease; data from the Phase 3 STRIDE-8 trial
evaluating CAPVAXIVE™ (Pneumococcal 21-valent Conjugate Vaccine) in
adults 18-64 years of age at increased risk of pneumococcal
disease; as well as a late-breaker oral presentation of Week 48
data from the Phase 2 study evaluating an investigational
once-weekly oral combination regimen of islatravir, the company’s
nucleoside reverse transcriptase translocation inhibitor (NRTTI),
and Gilead’s lenacapavir, a first-in-class capsid inhibitor, for
treatment of people with HIV-1 infection.
“The breadth of innovative research we will showcase during
IDWeek 2024 is a testament to our ongoing commitment to advancing
science with the pursuit of addressing persisting global health
needs, such as RSV,” said Dr. Paula Annunziato, senior vice
president, infectious diseases and vaccines, Global Clinical
Development, Merck Research Laboratories. “We are proud of our
company’s longstanding legacy and continued momentum in helping to
treat and prevent a variety of potentially serious infectious
diseases for individuals around the world and across all stages of
life – from birth through older adulthood – and we look forward to
sharing these data.”
Key data from Merck’s portfolio and pipeline to be presented
during IDWeek 2024:
- First time data from the Phase 2b/3 study evaluating a single
dose of clesrovimab (MK-1654) administered to pre-term and
full-term infants (Abstract #166, Late Breaker Oral Abstract
Session: Respiratory Viruses Across All Ages);
- First presentation of results from the interim analysis of the
Phase 3 trial evaluating the safety and efficacy of clesrovimab
versus palivizumab in infants and children at increased risk for
severe RSV disease (Abstract #167, Late Breaker Oral Abstract
Session: Respiratory Viruses Across All Ages);
- First presentation of data from the Phase 3 STRIDE-8 trial
evaluating CAPVAXIVE in vaccine-naïve adults 18-64 years of age at
increased risk of pneumococcal disease (Abstract #45, Poster
Session: Adult Vaccines);
- Week 48 data from the Phase 2 study evaluating once-weekly oral
islatravir plus lenacapavir (Abstract #577, Late Breaker Oral
Abstract Session: What's Going Viral);
- Data from the SPECTRA (Study of Prescribing patterns and
Effectiveness of Ceftolozane/Tazobactam [C/T] Real-world Analysis)
study (multiple abstracts) and updates from the SMART (Study for
Monitoring Antimicrobial Resistance Trends) surveillance program
(multiple abstracts).
Details on abstracts listed above and additional key
abstracts for Merck:
RSV
A Phase 2b/3 Study to Evaluate the
Efficacy and Safety of an Investigational Respiratory Syncytial
Virus (RSV) Antibody, Clesrovimab, in Healthy Preterm and Full-Term
Infants. A. Sinha.
Abstract #166, Oral Abstract, Late Breaker
Abstract Session: Respiratory Viruses Across All Ages
Phase 3, Randomized, Controlled Trial
Evaluating Safety, Efficacy, and Pharmacokinetics (PK) of
Clesrovimab in Infants and Children at Increased Risk for Severe
Respiratory Syncytial Virus (RSV) Disease. O. Ramilo.
Abstract #167, Oral Abstract, Late Breaker
Abstract Session: Respiratory Viruses Across All Ages
Pneumococcal
A Phase 3, Randomized Trial Investigating
the Safety, Tolerability, and Immunogenicity of V116, an
Investigational Adult-Specific Pneumococcal Conjugate Vaccine, in
Pneumococcal Vaccine-Naïve Adults 18–64 Years of Age with Increased
Risk for Pneumococcal Disease. P. Scott.
Abstract #45, Poster Session: Adult
Vaccines
Disparities and Inequities in the Burden
of Pneumococcal Disease in US Adults. N. Cossrow.
Abstract #242, Poster Session: HAIs:
Device-Associated (CLABSI, CAUTI, VAP)
Quantifying the Impact of Introducing a
New Adult-Focused PCV in the United States. O. Sharomi.
Abstract #58, Poster Session: Adult
Vaccines
HIV
Week 48 Results of a Phase 2 Study
Evaluating Once-weekly Oral Islatravir Plus Lenacapavir. A.
Colson.
Abstract #577, Oral Abstract, Late Breaker
Abstract Session: What's Going Viral
Undesired Weight Gain and Associated
Healthcare Outcomes Among People with HIV on Antiretroviral
Treatment. B.K. Tadese.
Abstract #540, Poster Session: HIV:
Treatment
Antivirals
Drug-Drug Interactions (DDIs) with
Letermovir (LET) for Cytomegalovirus (CMV) Prophylaxis in Pediatric
(Birth to <18 Years of Age) Hematopoietic Cell Transplant (HCT)
Recipients. L. Danziger-Isakov.
Abstract #1196, Poster Session: Pediatric
Viral Studies
A SFGM-TC Real-world Study to Characterize
Pediatric Patients Undergoing Allogeneic Hematopoietic Stem Cell
Transplantation (HSCT) and Identify Both the Cytomegalovirus (CMV)
Serology Status of Both Recipients and Their Donors. X. Bourge.
Abstract #2356, Poster Session: Virology:
Epidemiology of Viral Infections
Virologic and Clinical Outcomes Among
Participants Hospitalized in a Phase 3 Trial Comparing Molnupiravir
with Placebo for Treating Mild-to-Moderate COVID-19. M.
Johnson.
Abstract #1928, Poster Session: COVID-19:
Complications, Coinfections and Clinical Outcomes
Antibiotics
Treatment Patterns Among Hospitalized
Patients with Gram-Negative Infection Treated with
Imipenem/Cilastatin/Relebactam (I/R): Retrospective US-Based EHR
Medical Chart Review. E. Yucel.
Abstract #1075, Poster Session: Novel
Agents
Effectiveness of Imipenem-Relebactam for
Multidrug-resistant Pseudomonas AeruGinosa in PnEumonia and
Bloodstream Infections in the United States (MIRAGE): Preliminary
Results. R. Shields.
Abstract #1105, Poster Session: Novel
Agents
Comparative Effectiveness of Early
Treatment with Ceftolozane/Tazobactam (C/T) Relative to Polymyxin
(PB)-based Therapy for Non-COVID-19 Patients (pts) with Pneumonia
(PNA) due to Multi-drug Resistant Pseudomonas Aeruginosa (MDR-PSA)
Across US Hospitals. T. Lodise.
Abstract #1537, Poster Session: Treatment
of Antimicrobial Resistant Infections
Clinical Outcomes in Patients Hospitalized
with Exacerbation of Chronic Respiratory Infections Treated with
Ceftolozane/Tazobactam: Results from SPECTRA. E. Yucel.
Abstract #1074, Poster Session: Novel
Agents
Describing the Clinical Characteristics,
Treatment Patterns and Outcomes in Hospitalized Pneumonia Patients
Treated with Ceftolozane/Tazobactam (C/T): Insights from the
SPECTRA Study. E. Yucel.
Abstract #1076, Poster Session: Novel
Agents
Treatment Patterns and Clinical Outcomes
in Hospitalized Patients with Febrile Neutropenia Treated with
Ceftolozane/Tazobactam: A Subgroup Analysis of the SPECTRA Study.
E. Yucel.
Abstract #1113, Poster Session: Novel
Agents
Study of Prescribing patterns and
Effectiveness of Ceftolozane/Tazobactam [C/T) Real-world Analysis
Results (SPECTRA): Results of Immunocompromised Patients. E.
Yucel.
Abstract #2305, Poster Session:
Transplant: Studies of Empiric and Preemptive Therapy
Study of Prescribing patterns and
Effectiveness of Ceftolozane/Tazobactam (C/T) Real-world Analysis
(SPECTRA): Clinical Outcomes and Treatment Patterns from Mexico. E.
Yucel.
Abstract #1077, Poster Session: Novel
Agents
Antimicrobial
Epidemiology/Surveillance
Susceptibility of Clinical
Non-Morganellaceae Enterobacterales Isolates from Bloodstream and
Respiratory Tract Infections to Imipenem/Relebactam and
Comparators: SMART United States 2020-2022. M. Wise.
Abstract #1519, Poster Session: Treatment
of Antimicrobial Resistant Infections
Activity of Ceftolozane/Tazobactam,
Imipenem/Relebactam and Comparators Against Clinical MDR and DTR
non-Morganellaceae Enterobacterales and Pseudomonas Aeruginosa
Stratified by Patient Age and Hospital Ward: SMART United States
2020-2022. M. Wise.
Abstract #1518, Poster Session: Treatment
of Antimicrobial Resistant Infections
About Clesrovimab (MK-1654)
Clesrovimab (MK-1654) is an investigational, extended half-life
monoclonal antibody (mAb) developed as a passive immunization for
the prevention of RSV. Clesrovimab is designed to be administered
as the same single dose, regardless of birth weight, and is being
studied in healthy pre-term, full-term and at-risk infants to
provide direct, rapid and durable protection through their first
RSV season against mild, moderate and severe RSV.
About CAPVAXIVE
CAPVAXIVE is Merck’s approved 21-valent pneumococcal conjugate
vaccine indicated for active immunization for the prevention of
invasive disease and pneumonia in adults 18 years of age and older.
CAPVAXIVE is specifically designed to help address Streptococcus
pneumoniae serotypes predominantly responsible for adult invasive
pneumococcal disease (IPD), including eight unique serotypes, 15A,
15C, 16F, 23A, 23B, 24F, 31, and 35B compared to other pneumococcal
vaccines. CAPVAXIVE is administered as a single dose.
Select Safety Information for CAPVAXIVE
Do not administer CAPVAXIVE to individuals with a history of a
severe allergic reaction (eg, anaphylaxis) to any component of
CAPVAXIVE or to diphtheria toxoid.
Individuals with altered immunocompetence, including those
receiving immunosuppressive therapy, may have a reduced immune
response to CAPVAXIVE.
The most commonly reported (>10%) solicited adverse reactions
in individuals 18 through 49 years of age who received CAPVAXIVE
were: injection-site pain (73.1%), fatigue (36.0%), headache
(27.5%), myalgia (16.4%), injection-site erythema (13.8%), and
injection-site swelling (13.3%).
The most commonly reported (>10%) solicited adverse reactions
in individuals 50 years of age and older who received CAPVAXIVE
were: injection-site pain (41.2%), fatigue (19.7%), and headache
(11.0%).
Vaccination with CAPVAXIVE may not protect all vaccine
recipients.
Authorized Use of LAGEVRIO™ (molnupiravir) in the
U.S.
LAGEVRIO (molnupiravir) is authorized for use under an Emergency
Use Authorization (EUA) for the treatment of adults with
mild-to-moderate coronavirus disease 2019 (COVID-19):
- who are at high risk for progression to severe COVID-19,
including hospitalization or death, and
- for whom alternative COVID-19 treatment options approved or
authorized by FDA are not accessible or clinically
appropriate.
LAGEVRIO is not approved for any use, including the treatment of
COVID-19, but is authorized for emergency use by the FDA under an
Emergency Use Authorization (EUA).
The emergency use of LAGEVRIO is only authorized for the
duration of the declaration that circumstances exist justifying the
authorization of the emergency use of drugs and biological products
during the COVID-19 pandemic under Section 564(b)(1) of the Federal
Food, Drug, and Cosmetic Act, 21 U.S.C. § 360bbb-3(b)(1) unless the
declaration is terminated or authorization revoked sooner.
Limitations of Authorized Use
LAGEVRIO is not authorized:
- for use in patients who are less than 18 years of age
- for initiation of treatment in patients hospitalized due to
COVID-19. Benefit of treatment with LAGEVRIO has not been observed
in subjects when treatment was initiated after hospitalization due
to COVID-19
- for use for longer than 5 consecutive days
- for pre-exposure or post-exposure prophylaxis for prevention of
COVID-19
LAGEVRIO may only be prescribed for an individual patient by
physicians, advanced practice registered nurses, and physician
assistants that are licensed or authorized under state law to
prescribe drugs in the therapeutic class to which LAGEVRIO belongs
(ie, anti-infectives).
Selected Safety Information for LAGEVRIO
Contraindications
No contraindications have been identified based on the limited
available data on the emergency use of LAGEVRIO authorized under
this EUA.
Warnings and Precautions
There are limited clinical data available for LAGEVRIO. Serious
and unexpected adverse events may occur that have not been
previously reported with LAGEVRIO use.
LAGEVRIO is not recommended for use during pregnancy. Based on
findings from animal reproduction studies, LAGEVRIO may cause fetal
harm when administered to pregnant individuals. There are no
available human data on the use of LAGEVRIO in pregnant individuals
to evaluate the risk of major birth defects, miscarriage, or
adverse maternal or fetal outcomes.
LAGEVRIO is authorized to be prescribed to a pregnant individual
only after the healthcare provider has determined that the benefits
would outweigh the risks for that individual patient. If the
decision is made to use LAGEVRIO during pregnancy, the prescribing
healthcare provider must document that the known and potential
benefits and the potential risks of using LAGEVRIO during pregnancy
were communicated to the pregnant individual.
There is a pregnancy registry that monitors pregnancy outcomes
in individuals exposed to LAGEVRIO during pregnancy. The
prescribing healthcare provider must document that a pregnant
individual was made aware of the pregnancy registry at
https://covid-pr.pregistry.com or 1-800-616-3791. Pregnant
individuals exposed to LAGEVRIO or their healthcare providers can
also report the exposure by contacting Merck Sharp & Dohme LLC,
Rahway, NJ, USA at 1-877-888-4231.
Advise individuals of childbearing potential of the potential
risk to a fetus and to use an effective method of contraception
correctly and consistently during treatment with LAGEVRIO and for 4
days after the final dose.
Prior to initiating treatment with LAGEVRIO, assess whether an
individual of childbearing potential is pregnant or not, if
clinically indicated.
Hypersensitivity reactions, including anaphylaxis, have been
reported with LAGEVRIO. If signs and symptoms of a clinically
significant hypersensitivity reaction or anaphylaxis occur,
immediately discontinue LAGEVRIO and initiate appropriate
medications and/or supportive care.
LAGEVRIO is not authorized for use in patients less than 18
years of age because it may affect bone and cartilage growth. The
safety and efficacy of LAGEVRIO have not been established in
pediatric patients.
Adverse Reactions
The most common adverse reactions occurring in ≥1% of subjects
in the LAGEVRIO treatment group in the Phase 3 double-blind
MOVe-OUT study were diarrhea (2% versus placebo at 2%), nausea (1%
versus placebo at 1%), and dizziness (1% versus placebo at 1%) all
of which were Grade 1 (mild) or Grade 2 (moderate).
Serious adverse events occurred in 7% of subjects receiving
LAGEVRIO and 10% receiving placebo; most serious adverse events
were COVID-19 related. Adverse events leading to death occurred in
2 (<1%) of the subjects receiving LAGEVRIO and 12 (2%) of
subjects receiving placebo.
Drug Interactions
No drug interactions have been identified based on the limited
available data on the emergency use of LAGEVRIO. No clinical
drug-drug interaction trials of LAGEVRIO with concomitant
medications, including other treatments for mild-to-moderate
COVID-19, have been conducted.
Pregnancy/Breastfeeding
There are no data on the presence of molnupiravir or its
metabolites in human milk. It is unknown whether molnupiravir has
an effect on the breastfed infant or effects on milk production.
Based on the potential for adverse reactions in the infant from
LAGEVRIO, breastfeeding is not recommended during treatment with
LAGEVRIO and for 4 days after the final dose. A lactating
individual may consider interrupting breastfeeding and may consider
pumping and discarding breast milk during treatment and for 4 days
after the last dose of LAGEVRIO.
Males of Reproductive Potential
While the risk is regarded as low, there is a theoretical risk
for LAGEVRIO to affect offspring of treated males based on its
mechanism of action. Advise sexually active individuals with
partners of childbearing potential to use a reliable method of
contraception correctly and consistently during treatment and for
at least 3 months after the last dose of LAGEVRIO. The risk beyond
three months after the last dose of LAGEVRIO is unknown.
Required Reporting for Serious Adverse Events and Medication
Errors
The prescribing healthcare provider and/or the provider’s
designee is/are responsible for mandatory reporting of all serious
adverse events and medication errors potentially related to
LAGEVRIO within 7 calendar days from the healthcare provider’s
awareness of the event.
Submit adverse event and medication error reports, using FDA
Form 3500, to FDA MedWatch using one of the following methods:
Complete and submit the report online:
www.fda.gov/medwatch/report.htm
- Complete and submit a postage-paid FDA Form 3500
(https://www.fda.gov/media/76299/download) and return by:
- Mail to MedWatch, 5600 Fishers Lane, Rockville, MD 20852-9787,
or
- Fax to 1-800-FDA-0178, or
- Call 1-800-FDA-1088 to request a reporting form
In addition, please provide a copy of all FDA MedWatch forms
to:
Merck Sharp & Dohme LLC, Rahway, NJ, USA by:
- Fax: 215-616-5677
- Email: dpoc.usa@merck.com
Indications for PREVYMIS® (letermovir)
PREVYMIS is indicated for prophylaxis of cytomegalovirus (CMV)
infection and disease in adult and pediatric patients 6 months of
age and older and weighing at least 6 kg who are CMV-seropositive
recipients [R+] of an allogeneic hematopoietic stem cell transplant
(HSCT).
PREVYMIS is indicated for prophylaxis of CMV disease in adult
and pediatric patients 12 years of age and older and weighing at
least 40 kg who are kidney transplant recipients at high risk
(Donor CMV seropositive/Recipient CMV seronegative [D+/R-]).
Selected Safety Information for PREVYMIS
Contraindications
PREVYMIS is contraindicated in patients receiving pimozide or
ergot alkaloids.
- Increased pimozide concentrations may lead to QT prolongation
and torsades de pointes.
- Increased ergot alkaloids concentrations may lead to
ergotism.
PREVYMIS is contraindicated with pitavastatin and simvastatin
when co-administered with cyclosporine. Significantly increased
pitavastatin or simvastatin concentrations may lead to myopathy or
rhabdomyolysis.
Warnings and Precautions
The concomitant use of PREVYMIS and certain drugs may result in
potentially significant drug interactions, some of which may lead
to adverse reactions (PREVYMIS or concomitant drugs) or reduced
therapeutic effect of PREVYMIS or the concomitant drug.
Intravenous formulation of PREVYMIS contains the excipient
hydroxypropyl betadex. PREVYMIS injection should be used only in
patients unable to take oral therapy and patients should be
switched to oral PREVYMIS as soon as they are able to take oral
medications. If possible, intravenous administration should not
exceed 4 weeks.
In patients with renal impairment, accumulation of hydroxypropyl
betadex may occur. In adult patients with CLcr less than 50 mL/min
and in pediatric patients with a similar degree of renal impairment
(based on age-appropriate assessment of renal function) receiving
PREVYMIS injection, closely monitor serum creatinine levels.
Animal studies have shown the potential for hydroxypropyl
betadex to cause ototoxicity. The active ingredient, letermovir, is
not known to be associated with ototoxicity.
Adverse Reactions
The rate of adverse events occurring in at least 10% of adult
HSCT recipients treated with PREVYMIS and at a frequency at least
2% greater than placebo were nausea (27% vs 23%), diarrhea (26% vs
24%), vomiting (19% vs 14%), peripheral edema (14% vs 9%), cough
(14% vs 10%), headache (14% vs 9%), fatigue (13% vs 11%), and
abdominal pain (12% vs 9%).
Hypersensitivity reaction, with associated moderate dyspnea,
occurred in one adult HSCT recipient following the first infusion
of IV PREVYMIS after switching from oral PREVYMIS, leading to
treatment discontinuation.
The most common adverse event occurring in at least 10% of adult
kidney transplant recipients treated with PREVYMIS and at a
frequency greater than valganciclovir was diarrhea (32% vs
29%).
The safety profile of PREVYMIS in pediatric subjects was
consistent with the safety profile observed in clinical trials of
PREVYMIS in adults.
Drug Interactions
If PREVYMIS is co-administered with cyclosporine, the dosage of
PREVYMIS should be decreased to 240 mg once daily in adult and
pediatric patients 12 years of age and older. If PREVYMIS is
co-administered with cyclosporine in pediatric patients less than
12 years of age, dose adjustment may be required.
Co-administration of PREVYMIS may alter the plasma
concentrations of other drugs and other drugs may alter the plasma
concentrations of PREVYMIS. Consult the full Prescribing
Information prior to and during treatment for potential drug
interactions.
Closely monitor serum creatinine levels in patients with CLcr
less than 50 mL/min using PREVYMIS injection.
PREVYMIS is not recommended for patients with severe (Child-Pugh
Class C) hepatic impairment.
Use in Specific Populations
The safety and effectiveness of PREVYMIS have not been
established for:
- HSCT recipients less than 6 months of age or weighing less than
6 kg, or
- Kidney transplant recipients less than 12 years of age or
weighing less than 40 kg.
For patients with creatinine clearance (CLcr) greater than 10
mL/min (by Cockcroft-Gault equation), no dosage adjustment of
PREVYMIS is required based on renal impairment. The safety of
PREVYMIS in patients with end-stage renal disease (CLcr less than
10 mL/min), including patients on dialysis, is unknown.
Following the completion of PREVYMIS prophylaxis, monitoring for
CMV reactivation in HSCT recipients is recommended.
Indications and usage for RECARBRIO™ (imipenem, cilastatin,
and relebactam)
RECARBRIO is indicated for the treatment of patients 18 years of
age and older with hospital-acquired bacterial pneumonia and
ventilator-associated bacterial pneumonia (HABP/VABP), caused by
the following susceptible gram-negative microorganisms:
Acinetobacter calcoaceticus-baumannii complex, Enterobacter
cloacae, Escherichia coli, Haemophilus influenzae, Klebsiella
aerogenes, Klebsiella oxytoca, Klebsiella pneumoniae, Pseudomonas
aeruginosa and Serratia marcescens.
RECARBRIO is indicated in patients 18 years of age and older who
have limited or no alternative treatment options, for the treatment
of complicated urinary tract infections (cUTI), including
pyelonephritis, caused by the following susceptible gram-negative
microorganisms: Enterobacter cloacae, Escherichia coli, Klebsiella
aerogenes, Klebsiella pneumoniae, and Pseudomonas aeruginosa.
RECARBRIO is indicated in patients 18 years of age and older who
have limited or no alternative treatment options for the treatment
of complicated intra-abdominal infections (cIAI) caused by the
following susceptible gram-negative microorganisms: Bacteroides
caccae, Bacteroides fragilis, Bacteroides ovatus, Bacteroides
stercoris, Bacteroides thetaiotaomicron, Bacteroides uniformis,
Bacteroides vulgatus, Citrobacter freundii, Enterobacter cloacae,
Escherichia coli, Fusobacterium nucleatum, Klebsiella aerogenes,
Klebsiella oxytoca, Klebsiella pneumoniae, Parabacteroides
distasonis, and Pseudomonas aeruginosa.
Approval of the cUTI and cIAI indications is based on limited
clinical safety and efficacy data for RECARBRIO.
Usage
To reduce the development of drug-resistant bacteria and
maintain the effectiveness of RECARBRIO and other antibacterial
drugs, RECARBRIO should be used only to treat or prevent infections
that are proven or strongly suspected to be caused by susceptible
bacteria. When culture and susceptibility information are
available, they should be considered in selecting or modifying
antibacterial therapy. In the absence of such data, local
epidemiology and susceptibility patterns may contribute to the
empiric selection of therapy.
Selected Safety Information for RECARBRIO
Hypersensitivity Reactions: RECARBRIO is contraindicated
in patients with a history of known severe hypersensitivity (severe
systemic allergic reaction such as anaphylaxis) to any component of
RECARBRIO. Serious and occasionally fatal hypersensitivity
(anaphylactic) reactions have been reported in patients receiving
therapy with beta-lactams. Before initiating therapy with
RECARBRIO, careful inquiry should be made concerning previous
hypersensitivity reactions to carbapenems, penicillins,
cephalosporins, other beta-lactams, and other allergens. If a
hypersensitivity reaction to RECARBRIO occurs, discontinue the
therapy immediately.
Seizures and Other Central Nervous System (CNS) Adverse
Reactions: CNS adverse reactions, such as seizures, confusional
states, and myoclonic activity, have been reported during treatment
with imipenem/cilastatin, a component of RECARBRIO, especially when
recommended dosages of imipenem were exceeded. These have been
reported most commonly in patients with CNS disorders (eg, brain
lesions or history of seizures) and/or compromised renal
function.
Anticonvulsant therapy should be continued in patients with
known seizure disorders. If CNS adverse reactions including
seizures occur, patients should undergo a neurological evaluation
to determine whether RECARBRIO should be discontinued.
Increased Seizure Potential Due to Interaction with Valproic
Acid: Concomitant use of RECARBRIO, with valproic acid or
divalproex sodium may increase the risk of breakthrough seizures.
Avoid concomitant use of RECARBRIO with valproic acid or divalproex
sodium or consider alternative antibacterial drugs other than
carbapenems.
Clostridioides difficile–Associated Diarrhea (CDAD) has
been reported with use of nearly all antibacterial agents,
including RECARBRIO, and may range in severity from mild diarrhea
to fatal colitis. Careful medical history is necessary since CDAD
has been reported to occur over two months after the administration
of antibacterial agents. If CDAD is suspected or confirmed, ongoing
antibacterial drug use not directed against C difficile may need to
be discontinued.
Development of Drug-Resistant Bacteria: Prescribing
RECARBRIO in the absence of a proven or strongly suspected
bacterial infection or prophylactic indication is unlikely to
provide benefit to the patient and increases the risk of the
development of drug-resistant bacteria.
Adverse Reactions: The most frequently reported adverse
reactions occurring in ≥5% of HABP/VABP patients treated with
RECARBRIO were aspartate aminotransferase increased (11.7%), anemia
(10.5%), alanine aminotransferase increased (9.8%), diarrhea
(7.9%), hypokalemia (7.9%), and hyponatremia (6.4%).
The most frequently reported adverse reactions occurring in ≥2%
of cUTI and cIAI patients treated with RECARBRIO were diarrhea
(6%), nausea (6%), headache (4%), vomiting (3%), alanine
aminotransferase increased (3%), aspartate aminotransferase
increased (3%), phlebitis/infusion site reactions (2%), pyrexia
(2%), and hypertension (2%).
Indications and usage for ZERBAXA® (ceftolozane and
tazobactam)
ZERBAXA is indicated for the treatment of adult patients (18
years and older) with hospital-acquired bacterial pneumonia and
ventilator-associated bacterial pneumonia (HABP/VABP), caused by
the following susceptible Gram-negative microorganisms:
Enterobacter cloacae, Escherichia coli, Haemophilus influenzae,
Klebsiella oxytoca, Klebsiella pneumoniae, Proteus mirabilis,
Pseudomonas aeruginosa, and Serratia marcescens.
ZERBAXA is indicated for the treatment of adult and pediatric
patients (birth to less than 18 years old) with complicated urinary
tract infections (cUTI), including pyelonephritis, caused by the
following susceptible Gram-negative microorganisms: Escherichia
coli, Klebsiella pneumoniae, Proteus mirabilis, and Pseudomonas
aeruginosa.
ZERBAXA used in combination with metronidazole is indicated for
the treatment of adult and pediatric patients (birth to less than
18 years old) with complicated intra-abdominal infections (cIAI)
caused by the following susceptible Gram-negative and Gram-positive
microorganisms: Enterobacter cloacae, Escherichia coli, Klebsiella
oxytoca, Klebsiella pneumoniae, Proteus mirabilis, Pseudomonas
aeruginosa, Bacteroides fragilis, Streptococcus anginosus,
Streptococcus constellatus, and Streptococcus salivarius.
Usage
To reduce the development of drug-resistant bacteria and
maintain the effectiveness of ZERBAXA and other antibacterial
drugs, ZERBAXA should be used only to treat or prevent infections
that are proven or strongly suspected to be caused by susceptible
bacteria. When culture and susceptibility information are
available, they should be considered in selecting or modifying
antibacterial therapy. In the absence of such data, local
epidemiology and susceptibility patterns may contribute to the
empiric selection of therapy.
Important Safety Information for ZERBAXA
Patients with renal impairment: Decreased efficacy of
ZERBAXA has been observed in patients with baseline CrCl of 30 to
<50 mL/min. In a clinical trial of adult patients, patients with
cIAIs with CrCl >50 mL/min had a clinical cure rate of 85.2%
when treated with ZERBAXA plus metronidazole vs 87.9% when treated
with meropenem. In the same trial, patients with CrCl 30 to <50
mL/min had a clinical cure rate of 47.8% when treated with ZERBAXA
plus metronidazole vs 69.2% when treated with meropenem. A similar
trend was also seen in the cUTI trial. Dose adjustment is required
for adult patients with CrCl 50 mL/min or less. All doses of
ZERBAXA are administered over 1 hour. Monitor CrCl at least daily
in patients with changing renal function and adjust the dose of
ZERBAXA accordingly.
Hypersensitivity: ZERBAXA is contraindicated in patients
with known serious hypersensitivity to the components of ZERBAXA
(ceftolozane/tazobactam), piperacillin/tazobactam, or other members
of the beta-lactam class. Serious and occasionally fatal
hypersensitivity (anaphylactic) reactions have been reported in
patients receiving beta-lactam antibacterials. Before initiating
therapy with ZERBAXA, make careful inquiry about previous
hypersensitivity reactions to cephalosporins, penicillins, or other
beta-lactams. If an anaphylactic reaction to ZERBAXA occurs,
discontinue use and institute appropriate therapy.
Clostridioides difficile-associated diarrhea (CDAD),
ranging from mild diarrhea to fatal colitis, has been reported with
nearly all systemic antibacterial agents, including ZERBAXA.
Careful medical history is necessary because CDAD has been reported
to occur more than 2 months after the administration of
antibacterial agents. If CDAD is confirmed, antibacterial use not
directed against C. difficile should be discontinued, if
possible.
Development of drug-resistant bacteria: Prescribing
ZERBAXA in the absence of a proven or strongly suspected bacterial
infection or a prophylactic indication is unlikely to provide
benefit to the patient and risks the development of drug-resistant
bacteria.
Adverse reactions in adult patients with HABP/VABP: The
most common adverse reactions occurring in ≥5% of adult patients
receiving ZERBAXA in the HABP/VABP trial were hepatic transaminase
increased (11.9%), renal impairment/renal failure (8.9%), and
diarrhea (6.4%).
Adverse reactions in adult patients with cIAI or cUTI:
The most common adverse reactions occurring in ≥5% of adult
patients receiving ZERBAXA in the cUTI and cIAI trials were
headache (5.8%) in the cUTI trial, and nausea (7.9%), diarrhea
(6.2%), and pyrexia (5.6%) in the cIAI trial.
Adverse reactions in pediatric patients with cIAI or
cUTI: The most common adverse reactions occurring in ≥7% of
pediatric patients receiving ZERBAXA in the cIAI trial were
diarrhea (17%), thrombocytosis (16%), pyrexia (13%), abdominal pain
(11%), vomiting (10%), increased aspartate aminotransferase (7%),
and anemia (7%). The most common adverse reactions occurring in ≥7%
of pediatric patients receiving ZERBAXA in the cUTI trial were
thrombocytosis (9%), leukopenia (8%), diarrhea (7%), and pyrexia
(7%).
Pediatric Use: There is insufficient information to
recommend dosage adjustment for pediatric patients younger than 18
years of age with cIAI and cUTI with eGFR 50 mL/min/1.73m2 or less.
ZERBAXA is not recommended in pediatric patients who have an eGFR
50 mL/min/1.73m2 or less. Pediatric patients born at term or
pre-term may not have an eGFR of 50 mL/min/1.73m2 or greater at
birth or within the first few months of life.
About Merck
At Merck, known as MSD outside of the United States and Canada,
we are unified around our purpose: We use the power of leading-edge
science to save and improve lives around the world. For more than
130 years, we have brought hope to humanity through the development
of important medicines and vaccines. We aspire to be the premier
research-intensive biopharmaceutical company in the world – and
today, we are at the forefront of research to deliver innovative
health solutions that advance the prevention and treatment of
diseases in people and animals. We foster a diverse and inclusive
global workforce and operate responsibly every day to enable a
safe, sustainable and healthy future for all people and
communities. For more information, visit www.merck.com and connect
with us on X (formerly Twitter), Facebook, Instagram, YouTube and
LinkedIn.
Forward-Looking Statement of Merck & Co., Inc., Rahway,
N.J., USA
This news release of Merck & Co., Inc., Rahway, N.J., USA
(the “company”) includes “forward-looking statements” within the
meaning of the safe harbor provisions of the U.S. Private
Securities Litigation Reform Act of 1995. These statements are
based upon the current beliefs and expectations of the company’s
management and are subject to significant risks and uncertainties.
There can be no guarantees with respect to pipeline candidates that
the candidates will receive the necessary regulatory approvals or
that they will prove to be commercially successful. If underlying
assumptions prove inaccurate or risks or uncertainties materialize,
actual results may differ materially from those set forth in the
forward-looking statements.
Risks and uncertainties include but are not limited to, general
industry conditions and competition; general economic factors,
including interest rate and currency exchange rate fluctuations;
the impact of pharmaceutical industry regulation and health care
legislation in the United States and internationally; global trends
toward health care cost containment; technological advances, new
products and patents attained by competitors; challenges inherent
in new product development, including obtaining regulatory
approval; the company’s ability to accurately predict future market
conditions; manufacturing difficulties or delays; financial
instability of international economies and sovereign risk;
dependence on the effectiveness of the company’s patents and other
protections for innovative products; and the exposure to
litigation, including patent litigation, and/or regulatory
actions.
The company undertakes no obligation to publicly update any
forward-looking statement, whether as a result of new information,
future events or otherwise. Additional factors that could cause
results to differ materially from those described in the
forward-looking statements can be found in the company’s Annual
Report on Form 10-K for the year ended December 31, 2023 and the
company’s other filings with the Securities and Exchange Commission
(SEC) available at the SEC’s Internet site (www.sec.gov).
Please see Prescribing Information for CAPVAXIVE
(Pneumococcal 21-valent Conjugate Vaccine) at
https://www.merck.com/product/usa/pi_circulars/c/capvaxive/capvaxive_pi.pdf
and Patient Information/Medication Guide for CAPVAXIVE at
https://www.merck.com/product/usa/pi_circulars/c/capvaxive/capvaxive_ppi.pdf
Before prescribing LAGEVRIO (molnupiravir) please read the
Fact Sheet for Healthcare Providers, including Mandatory
Requirements for Administration of Molnupiravir under Emergency Use
Authorization, at
https://www.merck.com/eua/molnupiravir-hcp-fact-sheet.pdf
and Fact Sheet for Patients and Caregivers at
https://www.merck.com/eua/molnupiravir-patient-fact-sheet-english.pdf
Please see Prescribing Information for PREVYMIS (letermovir)
at
https://www.merck.com/product/usa/pi_circulars/p/prevymis/prevymis_pi.pdf,
Patient Information/Medication Guide for PREVYMIS at
https://www.merck.com/product/usa/pi_circulars/p/prevymis/prevymis_ppi.pdf
and Instructions for Use for PREVYMIS at
https://www.merck.com/product/usa/pi_circulars/p/prevymis/prevymis_ifu.pdf
Please see Prescribing Information for RECARBRIO (imipenem,
cilastatin, and relebactam) at
https://www.merck.com/product/usa/pi_circulars/r/recarbrio/recarbrio_pi.pdf
Please see Prescribing Information for ZERBAXA (ceftolozane
and tazobactam) at
https://www.merck.com/product/usa/pi_circulars/z/zerbaxa/zerbaxa_pi.pdf
View source
version on businesswire.com: https://www.businesswire.com/news/home/20241009405039/en/
Media Contacts:
Julie Cunningham (617) 519-6264
Courtney Ronaldo (908) 442-5695
Investor Contacts:
Peter Dannenbaum (732) 594-1579
Alexis Constantine (732) 594-1578
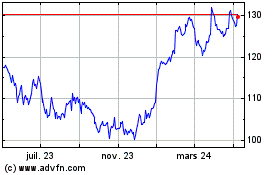
Merck (NYSE:MRK)
Graphique Historique de l'Action
De Nov 2024 à Déc 2024
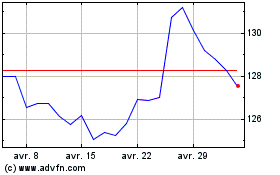
Merck (NYSE:MRK)
Graphique Historique de l'Action
De Déc 2023 à Déc 2024