First breakthrough therapy designation for
investigational sac-TMT in the U.S.
Merck (NYSE: MRK), known as MSD outside of the United States and
Canada, today announced that the U.S. Food and Drug Administration
(FDA) has granted Breakthrough Therapy designation to sacituzumab
tirumotecan (sac-TMT) for the treatment of patients with advanced
or metastatic nonsquamous non-small cell lung cancer (NSCLC) with
epidermal growth factor receptor (EGFR) mutations (exon 19 deletion
[19del] or exon 21 L858R) whose disease progressed on or after
tyrosine kinase inhibitor (TKI) and platinum-based chemotherapy.
Sac-TMT is an investigational trophoblast cell-surface antigen 2
(TROP2)-directed antibody drug conjugate (ADC) being developed in
collaboration with Kelun-Biotech. This designation is based on data
from the Phase 2 expansion cohort of a Phase 1/2 study evaluating
sac-TMT in patients with EGFR-mutated NSCLC, which were presented
at the 2023 American Society of Clinical Oncology Annual Meeting,
as well as data from two parts of a Phase 2 study evaluating
sac-TMT in patients with EGFR-mutated NSCLC who have been treated
with at least two lines of prior therapy.
“This designation by the FDA highlights the importance of
developing novel therapeutic options for patients living with
EGFR-mutated nonsquamous non-small cell lung cancer,” said Dr. Scot
Ebbinghaus, vice president, global clinical development, Merck
Research Laboratories. “We believe ADCs are an important modality
in the treatment of cancer and are rapidly advancing the clinical
development of sacituzumab tirumotecan, with the goal of
meaningfully improving upon current standards of care in certain
cancers.”
The FDA’s Breakthrough Therapy designation is granted to
expedite the development and review of medicines that are intended
to treat serious or life-threatening conditions. To qualify for
this designation, preliminary clinical evidence must indicate that
the product may demonstrate substantial improvement over currently
available options on at least one clinically significant endpoint.
The benefits of this Breakthrough Therapy Designation include more
intensive guidance from the FDA on an efficient development
program, access to a scientific liaison to help accelerate review
time and potential eligibility for Priority Review if relevant
criteria are met.
Merck is rapidly advancing the global clinical development
program evaluating sac-TMT as a monotherapy and in combination with
KEYTRUDA® (pembrolizumab) with 10 ongoing Phase 3 studies across
various solid tumors. Two of these ongoing trials include
TroFuse-004, which is evaluating sac-TMT versus chemotherapy
(docetaxel or pemetrexed) in patients with previously treated NSCLC
with EGFR mutations or other genomic alterations, and TroFuse-009
which is evaluating sac-TMT versus doublet chemotherapy (pemetrexed
and carboplatin) in certain patients with previously treated
EGFR-mutated NSCLC. These are the only Phase 3 trials evaluating a
TROP2 ADC in previously treated EGFR-mutated NSCLC.
Sac-TMT recently received its first marketing authorization in
China from the National Medical Products Administration (NMPA) for
the treatment of adult patients with unresectable locally advanced
or metastatic triple-negative breast cancer (TNBC) who have
received at least two prior systemic therapies (at least one of
which is for advanced or metastatic stage), based on results from
the Phase 3 OptiTROP-Breast01 study. Under a collaboration
agreement, Kelun-Biotech maintains the rights to develop,
manufacture and commercialize sac-TMT in Greater China (which
includes Mainland China, Hong Kong, Macau and Taiwan).
About sacituzumab tirumotecan (sac-TMT)
Sac-TMT is an investigational ADC that consists of three
components: 1) a TROP2-targeting monoclonal antibody, sacituzumab,
2) a cytotoxic payload from the topoisomerase 1 inhibitor class and
3) a novel, irreversible but hydrolyzable linker, which joins the
monoclonal antibody and the cytotoxic payload leveraging
proprietary linker conjugation technology. The average
drug-to-antibody ratio of sac-TMT is 7.4. TROP2 is highly expressed
in a variety of epithelial-derived tumors and can promote tumor
cell proliferation, invasion and metastasis. TROP2 ADCs
specifically target TROP2-expressing tumor cells to deliver
cytotoxic effects and have shown encouraging anti-tumor activity in
clinical studies.
Sac-TMT was developed by Kelun-Biotech. Kelun-Biotech (6990.HK)
is a holding subsidiary of Kelun Pharmaceutical (002422.SZ), which
focuses on the R&D, manufacturing, commercialization and global
collaboration of innovative biological drugs and small molecule
drugs. Under a collaboration agreement, Kelun-Biotech has granted
Merck the exclusive rights to develop, manufacture and
commercialize sac-TMT in all territories outside of Greater China
(which includes Mainland China, Hong Kong, Macau and Taiwan).
About lung cancer
Lung cancer is the leading cause of cancer death worldwide. In
2022 alone, there were approximately 2.4 million new cases and 1.8
million deaths from lung cancer globally. Non-small cell lung
cancer is the most common type of lung cancer, accounting for about
80% of all cases. Epidermal growth factor receptor mutations occur
in 14% to 38% of all NSCLC tumors worldwide. In 2024, the overall
five-year survival rate for patients diagnosed with lung cancer is
25% in the United States. Improved survival rates are due, in part,
to earlier detection and screening, reduction in smoking, advances
in diagnostic and surgical procedures, as well as the introduction
of new therapies. Early detection and screening remain an important
unmet need, as 44% of lung cancer cases are not found until they
are advanced.
Selected KEYTRUDA® (pembrolizumab) Indications in the
U.S.
Non-Small Cell Lung Cancer
KEYTRUDA, in combination with pemetrexed and platinum
chemotherapy, is indicated for the first-line treatment of patients
with metastatic nonsquamous non-small cell lung cancer (NSCLC),
with no EGFR or ALK genomic tumor aberrations.
KEYTRUDA, in combination with carboplatin and either paclitaxel
or paclitaxel protein-bound, is indicated for the first-line
treatment of patients with metastatic squamous NSCLC.
KEYTRUDA, as a single agent, is indicated for the first-line
treatment of patients with NSCLC expressing PD-L1 [Tumor Proportion
Score (TPS) ≥1%] as determined by an FDA-approved test, with no
EGFR or ALK genomic tumor aberrations, and is:
- Stage III where patients are not candidates for surgical
resection or definitive chemoradiation, or
- metastatic.
KEYTRUDA, as a single agent, is indicated for the treatment of
patients with metastatic NSCLC whose tumors express PD-L1 (TPS ≥1%)
as determined by an FDA-approved test, with disease progression on
or after platinum-containing chemotherapy. Patients with EGFR or
ALK genomic tumor aberrations should have disease progression on
FDA-approved therapy for these aberrations prior to receiving
KEYTRUDA.
KEYTRUDA is indicated for the treatment of patients with
resectable (tumors ≥4 cm or node positive) NSCLC in combination
with platinum-containing chemotherapy as neoadjuvant treatment, and
then continued as a single agent as adjuvant treatment after
surgery.
KEYTRUDA, as a single agent, is indicated as adjuvant treatment
following resection and platinum-based chemotherapy for adult
patients with Stage IB (T2a ≥4 cm), II, or IIIA NSCLC.
Selected Important Safety Information for KEYTRUDA
Severe and Fatal Immune-Mediated Adverse Reactions
KEYTRUDA is a monoclonal antibody that belongs to a class of
drugs that bind to either the programmed death receptor-1 (PD-1) or
the programmed death ligand 1 (PD-L1), blocking the PD-1/PD-L1
pathway, thereby removing inhibition of the immune response,
potentially breaking peripheral tolerance and inducing
immune-mediated adverse reactions. Immune-mediated adverse
reactions, which may be severe or fatal, can occur in any organ
system or tissue, can affect more than one body system
simultaneously, and can occur at any time after starting treatment
or after discontinuation of treatment. Important immune-mediated
adverse reactions listed here may not include all possible severe
and fatal immune-mediated adverse reactions.
Monitor patients closely for symptoms and signs that may be
clinical manifestations of underlying immune-mediated adverse
reactions. Early identification and management are essential to
ensure safe use of anti–PD-1/PD-L1 treatments. Evaluate liver
enzymes, creatinine, and thyroid function at baseline and
periodically during treatment. For patients with TNBC treated with
KEYTRUDA in the neoadjuvant setting, monitor blood cortisol at
baseline, prior to surgery, and as clinically indicated. In cases
of suspected immune-mediated adverse reactions, initiate
appropriate workup to exclude alternative etiologies, including
infection. Institute medical management promptly, including
specialty consultation as appropriate.
Withhold or permanently discontinue KEYTRUDA depending on
severity of the immune-mediated adverse reaction. In general, if
KEYTRUDA requires interruption or discontinuation, administer
systemic corticosteroid therapy (1 to 2 mg/kg/day prednisone or
equivalent) until improvement to Grade 1 or less. Upon improvement
to Grade 1 or less, initiate corticosteroid taper and continue to
taper over at least 1 month. Consider administration of other
systemic immunosuppressants in patients whose adverse reactions are
not controlled with corticosteroid therapy.
Immune-Mediated Pneumonitis
KEYTRUDA can cause immune-mediated pneumonitis. The incidence is
higher in patients who have received prior thoracic radiation.
Immune-mediated pneumonitis occurred in 3.4% (94/2799) of patients
receiving KEYTRUDA, including fatal (0.1%), Grade 4 (0.3%), Grade 3
(0.9%), and Grade 2 (1.3%) reactions. Systemic corticosteroids were
required in 67% (63/94) of patients. Pneumonitis led to permanent
discontinuation of KEYTRUDA in 1.3% (36) and withholding in 0.9%
(26) of patients. All patients who were withheld reinitiated
KEYTRUDA after symptom improvement; of these, 23% had recurrence.
Pneumonitis resolved in 59% of the 94 patients.
Pneumonitis occurred in 8% (31/389) of adult patients with cHL
receiving KEYTRUDA as a single agent, including Grades 3-4 in 2.3%
of patients. Patients received high-dose corticosteroids for a
median duration of 10 days (range: 2 days to 53 months).
Pneumonitis rates were similar in patients with and without prior
thoracic radiation. Pneumonitis led to discontinuation of KEYTRUDA
in 5.4% (21) of patients. Of the patients who developed
pneumonitis, 42% interrupted KEYTRUDA, 68% discontinued KEYTRUDA,
and 77% had resolution.
Pneumonitis occurred in 7% (41/580) of adult patients with
resected NSCLC who received KEYTRUDA as a single agent for adjuvant
treatment of NSCLC, including fatal (0.2%), Grade 4 (0.3%), and
Grade 3 (1%) adverse reactions. Patients received high-dose
corticosteroids for a median duration of 10 days (range: 1 day to
2.3 months). Pneumonitis led to discontinuation of KEYTRUDA in 26
(4.5%) of patients. Of the patients who developed pneumonitis, 54%
interrupted KEYTRUDA, 63% discontinued KEYTRUDA, and 71% had
resolution.
Immune-Mediated Colitis
KEYTRUDA can cause immune-mediated colitis, which may present
with diarrhea. Cytomegalovirus infection/reactivation has been
reported in patients with corticosteroid-refractory immune-mediated
colitis. In cases of corticosteroid-refractory colitis, consider
repeating infectious workup to exclude alternative etiologies.
Immune-mediated colitis occurred in 1.7% (48/2799) of patients
receiving KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (1.1%),
and Grade 2 (0.4%) reactions. Systemic corticosteroids were
required in 69% (33/48); additional immunosuppressant therapy was
required in 4.2% of patients. Colitis led to permanent
discontinuation of KEYTRUDA in 0.5% (15) and withholding in 0.5%
(13) of patients. All patients who were withheld reinitiated
KEYTRUDA after symptom improvement; of these, 23% had recurrence.
Colitis resolved in 85% of the 48 patients.
Hepatotoxicity and Immune-Mediated
Hepatitis
KEYTRUDA as a Single Agent
KEYTRUDA can cause immune-mediated hepatitis. Immune-mediated
hepatitis occurred in 0.7% (19/2799) of patients receiving
KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (0.4%), and Grade 2
(0.1%) reactions. Systemic corticosteroids were required in 68%
(13/19) of patients; additional immunosuppressant therapy was
required in 11% of patients. Hepatitis led to permanent
discontinuation of KEYTRUDA in 0.2% (6) and withholding in 0.3% (9)
of patients. All patients who were withheld reinitiated KEYTRUDA
after symptom improvement; of these, none had recurrence. Hepatitis
resolved in 79% of the 19 patients.
Immune-Mediated
Endocrinopathies
Adrenal Insufficiency
KEYTRUDA can cause primary or secondary adrenal insufficiency.
For Grade 2 or higher, initiate symptomatic treatment, including
hormone replacement as clinically indicated. Withhold KEYTRUDA
depending on severity. Adrenal insufficiency occurred in 0.8%
(22/2799) of patients receiving KEYTRUDA, including Grade 4
(<0.1%), Grade 3 (0.3%), and Grade 2 (0.3%) reactions. Systemic
corticosteroids were required in 77% (17/22) of patients; of these,
the majority remained on systemic corticosteroids. Adrenal
insufficiency led to permanent discontinuation of KEYTRUDA in
<0.1% (1) and withholding in 0.3% (8) of patients. All patients
who were withheld reinitiated KEYTRUDA after symptom
improvement.
Hypophysitis
KEYTRUDA can cause immune-mediated hypophysitis. Hypophysitis
can present with acute symptoms associated with mass effect such as
headache, photophobia, or visual field defects. Hypophysitis can
cause hypopituitarism. Initiate hormone replacement as indicated.
Withhold or permanently discontinue KEYTRUDA depending on severity.
Hypophysitis occurred in 0.6% (17/2799) of patients receiving
KEYTRUDA, including Grade 4 (<0.1%), Grade 3 (0.3%), and Grade 2
(0.2%) reactions. Systemic corticosteroids were required in 94%
(16/17) of patients; of these, the majority remained on systemic
corticosteroids. Hypophysitis led to permanent discontinuation of
KEYTRUDA in 0.1% (4) and withholding in 0.3% (7) of patients. All
patients who were withheld reinitiated KEYTRUDA after symptom
improvement.
Thyroid Disorders
KEYTRUDA can cause immune-mediated thyroid disorders.
Thyroiditis can present with or without endocrinopathy.
Hypothyroidism can follow hyperthyroidism. Initiate hormone
replacement for hypothyroidism or institute medical management of
hyperthyroidism as clinically indicated. Withhold or permanently
discontinue KEYTRUDA depending on severity. Thyroiditis occurred in
0.6% (16/2799) of patients receiving KEYTRUDA, including Grade 2
(0.3%). None discontinued, but KEYTRUDA was withheld in <0.1%
(1) of patients.
Hyperthyroidism occurred in 3.4% (96/2799) of patients receiving
KEYTRUDA, including Grade 3 (0.1%) and Grade 2 (0.8%). It led to
permanent discontinuation of KEYTRUDA in <0.1% (2) and
withholding in 0.3% (7) of patients. All patients who were withheld
reinitiated KEYTRUDA after symptom improvement. Hypothyroidism
occurred in 8% (237/2799) of patients receiving KEYTRUDA, including
Grade 3 (0.1%) and Grade 2 (6.2%). It led to permanent
discontinuation of KEYTRUDA in <0.1% (1) and withholding in 0.5%
(14) of patients. All patients who were withheld reinitiated
KEYTRUDA after symptom improvement. The majority of patients with
hypothyroidism required long-term thyroid hormone replacement. The
incidence of new or worsening hypothyroidism was higher in 1185
patients with HNSCC, occurring in 16% of patients receiving
KEYTRUDA as a single agent or in combination with platinum and FU,
including Grade 3 (0.3%) hypothyroidism. The incidence of new or
worsening hypothyroidism was higher in 389 adult patients with cHL
(17%) receiving KEYTRUDA as a single agent, including Grade 1
(6.2%) and Grade 2 (10.8%) hypothyroidism. The incidence of new or
worsening hyperthyroidism was higher in 580 patients with resected
NSCLC, occurring in 11% of patients receiving KEYTRUDA as a single
agent as adjuvant treatment, including Grade 3 (0.2%)
hyperthyroidism. The incidence of new or worsening hypothyroidism
was higher in 580 patients with resected NSCLC, occurring in 22% of
patients receiving KEYTRUDA as a single agent as adjuvant treatment
(KEYNOTE-091), including Grade 3 (0.3%) hypothyroidism.
Type 1 Diabetes Mellitus (DM), Which Can Present With Diabetic
Ketoacidosis
Monitor patients for hyperglycemia or other signs and symptoms
of diabetes. Initiate treatment with insulin as clinically
indicated. Withhold KEYTRUDA depending on severity. Type 1 DM
occurred in 0.2% (6/2799) of patients receiving KEYTRUDA. It led to
permanent discontinuation in <0.1% (1) and withholding of
KEYTRUDA in <0.1% (1) of patients. All patients who were
withheld reinitiated KEYTRUDA after symptom improvement.
Immune-Mediated Nephritis With Renal
Dysfunction
KEYTRUDA can cause immune-mediated nephritis. Immune-mediated
nephritis occurred in 0.3% (9/2799) of patients receiving KEYTRUDA,
including Grade 4 (<0.1%), Grade 3 (0.1%), and Grade 2 (0.1%)
reactions. Systemic corticosteroids were required in 89% (8/9) of
patients. Nephritis led to permanent discontinuation of KEYTRUDA in
0.1% (3) and withholding in 0.1% (3) of patients. All patients who
were withheld reinitiated KEYTRUDA after symptom improvement; of
these, none had recurrence. Nephritis resolved in 56% of the 9
patients.
Immune-Mediated Dermatologic Adverse
Reactions
KEYTRUDA can cause immune-mediated rash or dermatitis.
Exfoliative dermatitis, including Stevens-Johnson syndrome, drug
rash with eosinophilia and systemic symptoms, and toxic epidermal
necrolysis, has occurred with anti– PD-1/PD-L1 treatments. Topical
emollients and/or topical corticosteroids may be adequate to treat
mild to moderate nonexfoliative rashes. Withhold or permanently
discontinue KEYTRUDA depending on severity. Immune-mediated
dermatologic adverse reactions occurred in 1.4% (38/2799) of
patients receiving KEYTRUDA, including Grade 3 (1%) and Grade 2
(0.1%) reactions. Systemic corticosteroids were required in 40%
(15/38) of patients. These reactions led to permanent
discontinuation in 0.1% (2) and withholding of KEYTRUDA in 0.6%
(16) of patients. All patients who were withheld reinitiated
KEYTRUDA after symptom improvement; of these, 6% had recurrence.
The reactions resolved in 79% of the 38 patients.
Other Immune-Mediated Adverse
Reactions
The following clinically significant immune-mediated adverse
reactions occurred at an incidence of <1% (unless otherwise
noted) in patients who received KEYTRUDA or were reported with the
use of other anti–PD-1/PD-L1 treatments. Severe or fatal cases have
been reported for some of these adverse reactions.
Cardiac/Vascular: Myocarditis, pericarditis, vasculitis; Nervous
System: Meningitis, encephalitis, myelitis and demyelination,
myasthenic syndrome/myasthenia gravis (including exacerbation),
Guillain-Barré syndrome, nerve paresis, autoimmune neuropathy;
Ocular: Uveitis, iritis and other ocular inflammatory toxicities
can occur. Some cases can be associated with retinal detachment.
Various grades of visual impairment, including blindness, can
occur. If uveitis occurs in combination with other immune-mediated
adverse reactions, consider a Vogt-Koyanagi-Harada-like syndrome,
as this may require treatment with systemic steroids to reduce the
risk of permanent vision loss; Gastrointestinal: Pancreatitis, to
include increases in serum amylase and lipase levels, gastritis,
duodenitis; Musculoskeletal and Connective Tissue:
Myositis/polymyositis, rhabdomyolysis (and associated sequelae,
including renal failure), arthritis (1.5%), polymyalgia rheumatica;
Endocrine: Hypoparathyroidism; Hematologic/Immune: Hemolytic
anemia, aplastic anemia, hemophagocytic lymphohistiocytosis,
systemic inflammatory response syndrome, histiocytic necrotizing
lymphadenitis (Kikuchi lymphadenitis), sarcoidosis, immune
thrombocytopenic purpura, solid organ transplant rejection, other
transplant (including corneal graft) rejection.
Infusion-Related Reactions
KEYTRUDA can cause severe or life-threatening infusion-related
reactions, including hypersensitivity and anaphylaxis, which have
been reported in 0.2% of 2799 patients receiving KEYTRUDA. Monitor
for signs and symptoms of infusion-related reactions. Interrupt or
slow the rate of infusion for Grade 1 or Grade 2 reactions. For
Grade 3 or Grade 4 reactions, stop infusion and permanently
discontinue KEYTRUDA.
Complications of Allogeneic Hematopoietic Stem Cell
Transplantation (HSCT)
Fatal and other serious complications can occur in patients who
receive allogeneic HSCT before or after anti–PD-1/PD-L1 treatments.
Transplant- related complications include hyperacute
graft-versus-host disease (GVHD), acute and chronic GVHD, hepatic
veno-occlusive disease after reduced intensity conditioning, and
steroid-requiring febrile syndrome (without an identified
infectious cause). These complications may occur despite
intervening therapy between anti–PD-1/PD-L1 treatments and
allogeneic HSCT. Follow patients closely for evidence of these
complications and intervene promptly. Consider the benefit vs risks
of using anti–PD-1/PD-L1 treatments prior to or after an allogeneic
HSCT.
Increased Mortality in Patients With Multiple Myeloma
In trials in patients with multiple myeloma, the addition of
KEYTRUDA to a thalidomide analogue plus dexamethasone resulted in
increased mortality. Treatment of these patients with an
anti–PD-1/PD-L1 treatment in this combination is not recommended
outside of controlled trials.
Embryofetal Toxicity
Based on its mechanism of action, KEYTRUDA can cause fetal harm
when administered to a pregnant woman. Advise women of this
potential risk. In females of reproductive potential, verify
pregnancy status prior to initiating KEYTRUDA and advise them to
use effective contraception during treatment and for 4 months after
the last dose.
Adverse Reactions
In KEYNOTE-189, when KEYTRUDA was administered with pemetrexed
and platinum chemotherapy in metastatic nonsquamous NSCLC, KEYTRUDA
was discontinued due to adverse reactions in 20% of 405 patients.
The most common adverse reactions resulting in permanent
discontinuation of KEYTRUDA were pneumonitis (3%) and acute kidney
injury (2%). The most common adverse reactions (≥20%) with KEYTRUDA
were nausea (56%), fatigue (56%), constipation (35%), diarrhea
(31%), decreased appetite (28%), rash (25%), vomiting (24%), cough
(21%), dyspnea (21%), and pyrexia (20%).
In KEYNOTE-407, when KEYTRUDA was administered with carboplatin
and either paclitaxel or paclitaxel protein-bound in metastatic
squamous NSCLC, KEYTRUDA was discontinued due to adverse reactions
in 15% of 101 patients. The most frequent serious adverse reactions
reported in at least 2% of patients were febrile neutropenia,
pneumonia, and urinary tract infection. Adverse reactions observed
in KEYNOTE-407 were similar to those observed in KEYNOTE-189 with
the exception that increased incidences of alopecia (47% vs 36%)
and peripheral neuropathy (31% vs 25%) were observed in the
KEYTRUDA and chemotherapy arm compared to the placebo and
chemotherapy arm in KEYNOTE-407.
In KEYNOTE-042, KEYTRUDA was discontinued due to adverse
reactions in 19% of 636 patients with advanced NSCLC; the most
common were pneumonitis (3%), death due to unknown cause (1.6%),
and pneumonia (1.4%). The most frequent serious adverse reactions
reported in at least 2% of patients were pneumonia (7%),
pneumonitis (3.9%), pulmonary embolism (2.4%), and pleural effusion
(2.2%). The most common adverse reaction (≥20%) was fatigue
(25%).
In KEYNOTE-010, KEYTRUDA monotherapy was discontinued due to
adverse reactions in 8% of 682 patients with metastatic NSCLC; the
most common was pneumonitis (1.8%). The most common adverse
reactions (≥20%) were decreased appetite (25%), fatigue (25%),
dyspnea (23%), and nausea (20%).
In KEYNOTE-671, adverse reactions occurring in patients with
resectable NSCLC receiving KEYTRUDA in combination with
platinum-containing chemotherapy, given as neoadjuvant treatment
and continued as single-agent adjuvant treatment, were generally
similar to those occurring in patients in other clinical trials
across tumor types receiving KEYTRUDA in combination with
chemotherapy.
The most common adverse reactions (reported in ≥20%) in patients
receiving KEYTRUDA in combination with chemotherapy were
fatigue/asthenia, nausea, constipation, diarrhea, decreased
appetite, rash, vomiting, cough, dyspnea, pyrexia, alopecia,
peripheral neuropathy, mucosal inflammation, stomatitis, headache,
weight loss, abdominal pain, arthralgia, myalgia, insomnia, palmar-
plantar erythrodysesthesia, urinary tract infection, and
hypothyroidism.
In the neoadjuvant phase of KEYNOTE-671, when KEYTRUDA was
administered in combination with platinum-containing chemotherapy
as neoadjuvant treatment, serious adverse reactions occurred in 34%
of 396 patients. The most frequent (≥2%) serious adverse reactions
were pneumonia (4.8%), venous thromboembolism (3.3%), and anemia
(2%). Fatal adverse reactions occurred in 1.3% of patients,
including death due to unknown cause (0.8%), sepsis (0.3%), and
immune-mediated lung disease (0.3%). Permanent discontinuation of
any study drug due to an adverse reaction occurred in 18% of
patients who received KEYTRUDA in combination with
platinum-containing chemotherapy; the most frequent adverse
reactions (≥1%) that led to permanent discontinuation of any study
drug were acute kidney injury (1.8%), interstitial lung disease
(1.8%), anemia (1.5%), neutropenia (1.5%), and pneumonia
(1.3%).
Of the KEYTRUDA-treated patients who received neoadjuvant
treatment, 6% of 396 patients did not receive surgery due to
adverse reactions. The most frequent (≥1%) adverse reaction that
led to cancellation of surgery in the KEYTRUDA arm was interstitial
lung disease (1%).
In the adjuvant phase of KEYNOTE-671, when KEYTRUDA was
administered as a single agent as adjuvant treatment, serious
adverse reactions occurred in 14% of 290 patients. The most
frequent serious adverse reaction was pneumonia (3.4%). One fatal
adverse reaction of pulmonary hemorrhage occurred. Permanent
discontinuation of KEYTRUDA due to an adverse reaction occurred in
12% of patients who received KEYTRUDA as a single agent, given as
adjuvant treatment; the most frequent adverse reactions (≥1%) that
led to permanent discontinuation of KEYTRUDA were diarrhea (1.7%),
interstitial lung disease (1.4%), increased aspartate
aminotransferase (1%), and musculoskeletal pain (1%).
Adverse reactions observed in KEYNOTE-091 were generally similar
to those occurring in other patients with NSCLC receiving KEYTRUDA
as a single agent, with the exception of hypothyroidism (22%),
hyperthyroidism (11%), and pneumonitis (7%). Two fatal adverse
reactions of myocarditis occurred.
Lactation
Because of the potential for serious adverse reactions in
breastfed children, advise women not to breastfeed during treatment
and for 4 months after the last dose.
Merck’s focus on cancer
Every day, we follow the science as we work to discover
innovations that can help patients, no matter what stage of cancer
they have. As a leading oncology company, we are pursuing research
where scientific opportunity and medical need converge, underpinned
by our diverse pipeline of more than 25 novel mechanisms. With one
of the largest clinical development programs across more than 30
tumor types, we strive to advance breakthrough science that will
shape the future of oncology. By addressing barriers to clinical
trial participation, screening and treatment, we work with urgency
to reduce disparities and help ensure patients have access to
high-quality cancer care. Our unwavering commitment is what will
bring us closer to our goal of bringing life to more patients with
cancer. For more information, visit
https://www.merck.com/research/oncology.
About Merck
At Merck, known as MSD outside of the United States and Canada,
we are unified around our purpose: We use the power of leading-edge
science to save and improve lives around the world. For more than
130 years, we have brought hope to humanity through the development
of important medicines and vaccines. We aspire to be the premier
research-intensive biopharmaceutical company in the world – and
today, we are at the forefront of research to deliver innovative
health solutions that advance the prevention and treatment of
diseases in people and animals. We foster a diverse and inclusive
global workforce and operate responsibly every day to enable a
safe, sustainable and healthy future for all people and
communities. For more information, visit www.merck.com and connect
with us on X (formerly Twitter), Facebook, Instagram, YouTube and
LinkedIn.
Forward-Looking Statement of Merck & Co., Inc., Rahway,
N.J., USA
This news release of Merck & Co., Inc., Rahway, N.J., USA
(the “company”) includes “forward-looking statements” within the
meaning of the safe harbor provisions of the U.S. Private
Securities Litigation Reform Act of 1995. These statements are
based upon the current beliefs and expectations of the company’s
management and are subject to significant risks and uncertainties.
There can be no guarantees with respect to pipeline candidates that
the candidates will receive the necessary regulatory approvals or
that they will prove to be commercially successful. If underlying
assumptions prove inaccurate or risks or uncertainties materialize,
actual results may differ materially from those set forth in the
forward-looking statements.
Risks and uncertainties include but are not limited to, general
industry conditions and competition; general economic factors,
including interest rate and currency exchange rate fluctuations;
the impact of pharmaceutical industry regulation and health care
legislation in the United States and internationally; global trends
toward health care cost containment; technological advances, new
products and patents attained by competitors; challenges inherent
in new product development, including obtaining regulatory
approval; the company’s ability to accurately predict future market
conditions; manufacturing difficulties or delays; financial
instability of international economies and sovereign risk;
dependence on the effectiveness of the company’s patents and other
protections for innovative products; and the exposure to
litigation, including patent litigation, and/or regulatory
actions.
The company undertakes no obligation to publicly update any
forward-looking statement, whether as a result of new information,
future events or otherwise. Additional factors that could cause
results to differ materially from those described in the
forward-looking statements can be found in the company’s Annual
Report on Form 10-K for the year ended December 31, 2023 and the
company’s other filings with the Securities and Exchange Commission
(SEC) available at the SEC’s Internet site (www.sec.gov).
Please see Prescribing Information for KEYTRUDA
(pembrolizumab) at
http://www.merck.com/product/usa/pi_circulars/k/keytruda/keytruda_pi.pdf
and Medication Guide for KEYTRUDA at
http://www.merck.com/product/usa/pi_circulars/k/keytruda/keytruda_mg.pdf.
View source
version on businesswire.com: https://www.businesswire.com/news/home/20241203790598/en/
Media Contacts:
Julie Cunningham (617) 519-6264
Nikki Lupinacci (718) 644-0730
Investor Contacts:
Peter Dannenbaum (732) 594-1579
Damini Chokshi (732) 594-1577
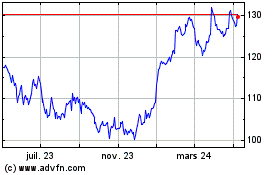
Merck (NYSE:MRK)
Graphique Historique de l'Action
De Nov 2024 à Déc 2024
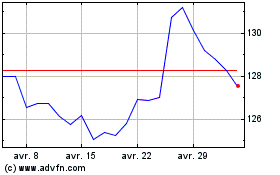
Merck (NYSE:MRK)
Graphique Historique de l'Action
De Déc 2023 à Déc 2024